Content warning
This story may contain sensitive material or discuss topics that some readers may find distressing. Reader discretion is advised. The views and opinions expressed in this story are those of the author and do not necessarily reflect the official policy or position of Vocal.

Introduction
Addiction has a huge impact on society in ways we are just beginning to understand, it's affecting individuals and communities in diverse ways. Traditionally it's associated with substance abuse, addiction manifests in various forms, ranging from compulsive shopping to disordered eating and problematic online pornography use (POPU). These addictive behaviors can disrupt lives, strain relationships, and undermine well-being, posing significant challenges to both individuals and the world at large.
No matter what addiction afflicts the individual, it still has the same damaging impact on the brain. For us to completely understand addiction we must uncover its many hidden forms. We must also call addiction out for what it truly is, a disease. This disease affects many people, leaving them feeling hopeless and in distress.
What is addiction?
I describe addiction as the "dis ease" of the brain. "Dis", the prefix, as seen in the word distant means far from. It could also refer to absence, reversal or "not functioning properly". Ease, the root word, describes a state of comfort and well being. So when putting them together you get far from comfort or far from well being. So with brain disease in mind, the brain is far from it's healthy state under these conditions. The departure from a state of ease or normal functioning, tells us all about the the disruptive nature of the disease on the brain's well-being.
Now we understand that the word "disease" typically refers to a specific medical condition or disorder that affects an organism, often involving abnormal functioning of the body or in this case the mind (which can effect the body). It implies a departure from a state of health or normal physiological functioning.
When observing the word addiction we notice the word add. This part of the word comes from the Latin word "addere," meaning "to give, bring to, or attach to." In the context of addiction, it implies attaching oneself to something.
According to the National Institute on Drug Abuse (NIDA), addiction is a chronic, relapsing disorder. It's a brain disorder that involves changes to brain circuits involved in reward , stress, and self-control.
The medical term used for addiction is substance use disorder. It's a treatable, chronic medical disease that involves complex interactions among brain circuits, genetics , the environment, and a person's life experiences.
People who are addicted to drugs or substances (addicts) are often called "dope heads" because they're always chasing after dopamine, a chemical in the brain that makes you feel good. It's likely that this term came from doctors who know about the science behind addiction and how dopamine affects it.
The Science
Addiction is an ongoing battle with the mind, a struggle that affects individuals across different forms of addictive behaviors. Regardless of the addiction, whether it's substance abuse, compulsive shopping, disordered eating, or problematic online pornography use, the impact on the brain remains consistent and damaging. The brain undergoes profound changes that make quitting very difficult.
At the heart of addiction lies dopamine, a neurotransmitter that serves as a key player in the brain's pleasure and reward system. Normally, the brain maintains a certain level of dopamine, but addictive substances or behaviors flood the brain with dopamine, creating a heightened sense of pleasure and euphoria. This flood of dopamine triggers a strong desire to repeat the behavior that caused it, leading to cravings and a relentless pursuit of that temporary high.
Dopamine also influences motivation, drive, and perception of time, further fueling the addictive cycle. Addicts find themselves driven by an insatiable craving for the pleasure they once experienced, often unaware of the time slipping away as they chase after their next fix.
Understanding this neurological aspect of addiction is crucial, as it highlights the challenges faced by individuals grappling with addictive behaviors. Breaking free from addiction requires adjusting the brain's chemistry and finding ways to replace short-lived euphoria with long-lasting rewards. However, for many addicts, this shift in perception proves to be a daunting task, this shows us the tight and pervasive grip addiction can have on one's life.
The Brain
Understanding the neuroscience of addiction involves exploring how the brain's reward system works, especially focusing on the key neurotransmitter dopamine. As previously stated, Dopamine plays a crucial role in shaping our behaviors and motivations.
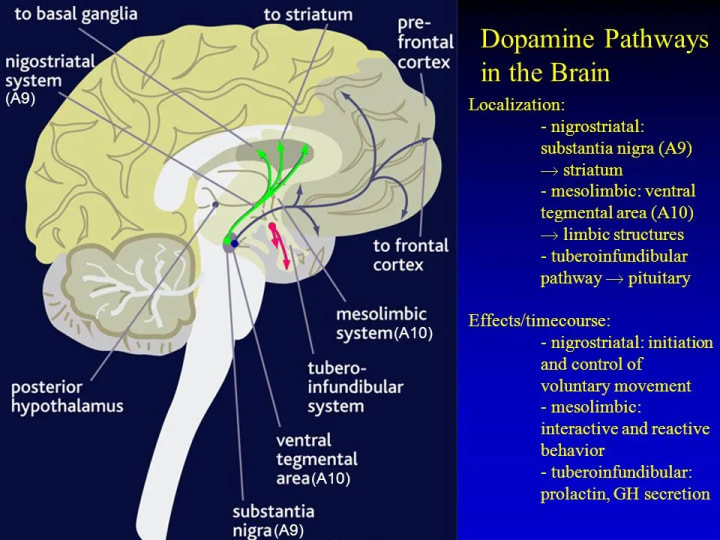
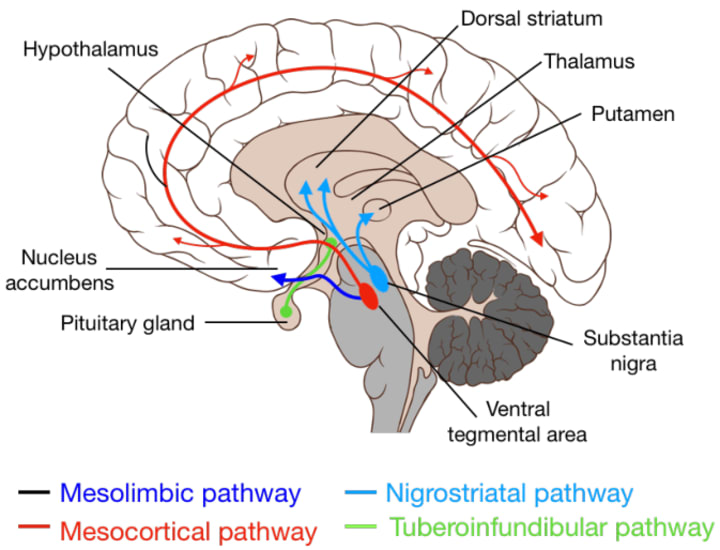
Imagine dopamine as a messenger in the brain, delivering signals that make us feel good when we do something enjoyable, like eating delicious food or spending time with loved ones. Dopamine operates through two main pathways: the reward pathway and the movement pathway.
Reward Pathway (mesocorticolimbic pathway): This pathway is like a highway in the brain that connects areas involved in experiencing pleasure and motivation. When we engage in activities that make us feel good, like eating our favorite dessert or winning a game, dopamine is released along this pathway, making us feel happy and motivated to repeat those activities.
Movement Pathway (nigrostriatal pathway): This pathway is more about physical movement. Dopamine helps control our ability to move smoothly and efficiently. It's like the conductor of an orchestra, coordinating different parts of the brain involved in movement.
Dopamine works with other chemicals in the brain, like glutamate, to carry out its effects. It can be released in two different ways:
Tonic Release: This is like a steady stream of dopamine, maintaining a baseline level of good feelings.
Phasic Release: This is like a sudden burst of dopamine, like when we get a surprise reward or experience something unexpectedly enjoyable.
But addiction throws this whole system out of balance. When someone becomes addicted to something, whether it's drugs, gambling, or even shopping, their brain's reward system gets hijacked. Instead of responding to normal, everyday pleasures, the brain becomes hyper-focused on the addictive substance or behavior. As a result...
Dopamine levels become dysregulated, with the brain craving more and more of the addictive substance or behavior to feel the same level of pleasure.
Motivation and drive become centered around obtaining the addictive substance or engaging in the addictive behavior, often at the expense of other important aspects of life.
Decision-making and impulse control, which are normally regulated by areas of the brain like the prefrontal cortex, are compromised. This makes it harder for someone to resist the urge to engage in addictive behaviors, even when they know it's harmful.
Additionally, when someone tries to quit an addiction, they often experience withdrawal symptoms. These symptoms can include low motivation, difficulty moving, and impaired decision-making, making it even harder to break free from the addictive cycle.
Addiction is like a glitch in the brain's reward system, causing it to prioritize addictive behaviors over everything else. Understanding this neuroscience helps us recognize the challenges people face when trying to overcome addiction and the importance of providing support and resources to help them on their journey to recovery.
Pathways in the Brain (Images)
Food Addiction
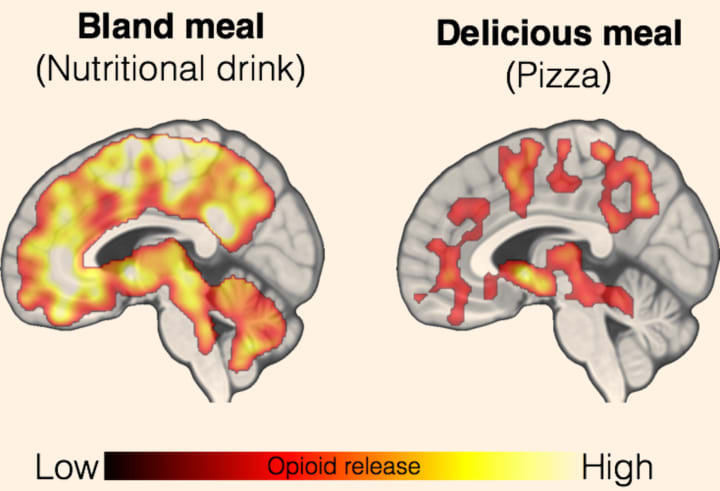
Food addiction is like when your body gets hooked on certain types of food, especially the ones that taste really good and have a lot of calories, like sugary snacks or fatty treats. Just like how people can get hooked on drugs, some folks can't seem to stop eating these kinds of foods, even when they know it's not good for them. This happens because of how our brains are wired to respond to these foods. When we eat something yummy, our brain releases dopamine.
When we eat a lot of these addictive foods, our bodies don't get all the good stuff they need, like vitamins and minerals. So, even though we're eating a lot of calories, our bodies are still hungry for the nutrients they're missing. This makes us feel hungry again much faster than if we ate healthier, nutrient-dense foods like fruits, veggies, and whole grains.
So, food addiction is a real thing, and it can make it really tough for some people to resist those tempting treats. But understanding how our brains and bodies respond to these foods can help us find ways to break free from food addiction and make healthier choices.
Shopping Addiction
Compulsive buying behavior (CBB), also known as shopping addiction, is a condition where individuals excessively and uncontrollably buy products despite negative consequences like financial problems and emotional distress. People with CBB often shop to improve their mood, cope with stress, or enhance their self-image, even though they may feel regretful afterward. This behavior is considered an addiction because it involves seeking pleasure and relief through shopping, which releases dopamine in the brain, just like drugs or food.
Research suggests that CBB shares common features with other behavioral addictions, such as high impulsivity, novelty seeking, and difficulty regulating emotions. People with CBB often have co-occurring psychiatric conditions like mood disorders, anxiety disorders, and substance use disorders.
Factors contributing to the development of CBB may include neurobiological abnormalities in regions of the brain involved in reward processing, as well as cultural factors like materialistic values and easy access to a wide variety of goods.
Studies have found that CBB is more prevalent in women and is often accompanied by high levels of psychopathology and personality traits like novelty seeking and harm avoidance.
Comparisons between CBB and other behavioral addictions like gambling disorder, internet gaming disorder, internet addiction, and sexual addiction highlight both similarities and differences in clinical profiles and personality traits.
Pornography Addiction
Porn addiction, like other forms of addiction, involves compulsive behavior despite negative consequences, loss of control over use, and withdrawal symptoms when unable to engage in the behavior. This behavioral addiction shares many similarities with substance addictions, particularly in its effects on the brain and behavior.
One of the key features of porn addiction is the overstimulation of the brain's reward system. When individuals repeatedly engage in watching pornography, they experience a surge of dopamine. This dopamine release reinforces the behavior, leading to a cycle of compulsive use to seek out the pleasurable experience again and again. Over time, this overstimulation can lead to desensitization, where individuals require more intense or novel stimuli to experience the same level of pleasure. This phenomenon is similar to tolerance seen in substance addiction, where individuals need increasing amounts of a substance to achieve the desired effect.
Neurobiological evidence supports the addictive nature of porn use, showing similarities with substance addiction in brain imaging studies. For example, individuals with porn addiction exhibit changes in brain activity and connectivity patterns, particularly in areas associated with reward processing and impulse control. These changes include sensitization, where the brain becomes hypersensitive to pornographic cues, and desensitization, where the brain's response to these cues diminishes over time. This dysregulation of the brain's reward system can contribute to compulsive and uncontrollable porn use, despite negative consequences such as relationship problems, decreased libido, and sexual dysfunction.
Porn addiction can have significant effects on psychological well-being and behavior. Individuals may experience psychosexual dissatisfaction, including sexual dysfunction and dissatisfaction with real-life sexual experiences. This dissatisfaction may stem from unrealistic expectations set by pornographic material, leading to performance anxiety and relationship difficulties. Additionally, porn addiction may be associated with comorbidities such as anxiety, depression, and substance abuse disorders, further complicating the clinical picture.
Alcohol Abuse
This addiction, known as Alcohol Use Disorder (AUD), ranges from mild to severe and can severely impact an individual's life.
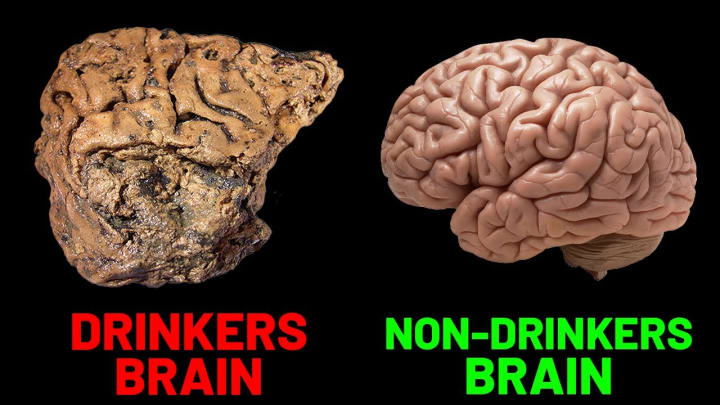
The brain plays a central role in alcohol addiction. Initially, alcohol can produce pleasurable feelings and reduce negative emotions, driving repeated consumption. Over time, progressive changes occur in the brain's structure and function, making it challenging to control alcohol use and leading to a cycle of addiction.
The addiction cycle consists of three stages: binge/intoxication, negative affect/withdrawal, and preoccupation/anticipation. During the binge stage, alcohol's rewarding effects reinforce drinking behavior, leading to habit formation. In the withdrawal stage, individuals experience negative symptoms when they stop drinking, driving them to consume alcohol to escape unpleasant feelings. In the preoccupation stage, cravings and impulsivity dominate as individuals seek alcohol again.
These stages are associated with changes in key brain regions, including the basal ganglia, extended amygdala, and prefrontal cortex. The basal ganglia reinforce alcohol consumption, while the extended amygdala contributes to stress and negative emotions. The prefrontal cortex, responsible for decision-making, is compromised, leading to impaired executive function.
Alcohol addiction can have severe consequences, including health issues, accidents, and social problems. Young people are especially vulnerable to AUD due to its impact on brain development. However, effective treatments, including behavioral therapies and medications, can help individuals recover from AUD at any age.
Substance Abuse
Nicotine, the primary addictive substance in tobacco products, acts as a stimulant in the brain. When nicotine is inhaled or absorbed into the bloodstream through smoking, it quickly reaches the brain where it binds to nicotinic acetylcholine receptors. This binding triggers the release of neurotransmitters such as dopamine, serotonin, and norepinephrine. Dopamine, in particular, plays a crucial role in the brain's reward system, reinforcing the behavior of smoking. The release of dopamine creates pleasurable sensations, which contributes to the addictive properties of nicotine.
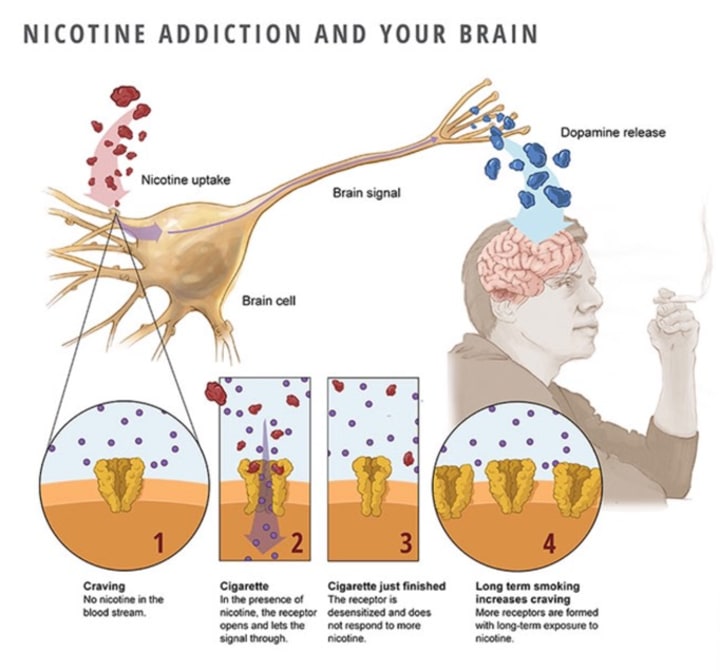
Over time, repeated exposure to nicotine leads to changes in the brain's reward system, making it increasingly difficult for individuals to quit smoking without experiencing withdrawal symptoms.
Amphetamines, including drugs like methamphetamine, work by increasing the release of neurotransmitters such as dopamine, serotonin, and norepinephrine. Methamphetamine, for example, enters the brain and causes the release of large amounts of dopamine from nerve terminals in the brain's reward system. This flood of dopamine produces intense feelings of euphoria, increased energy, and heightened alertness. The rapid and significant increase in dopamine levels reinforces drug-seeking behavior, leading to addiction. Chronic use of amphetamines can lead to long-term changes in the brain, including alterations in dopamine receptors and neurotransmitter levels, which contribute to addiction and dependence.
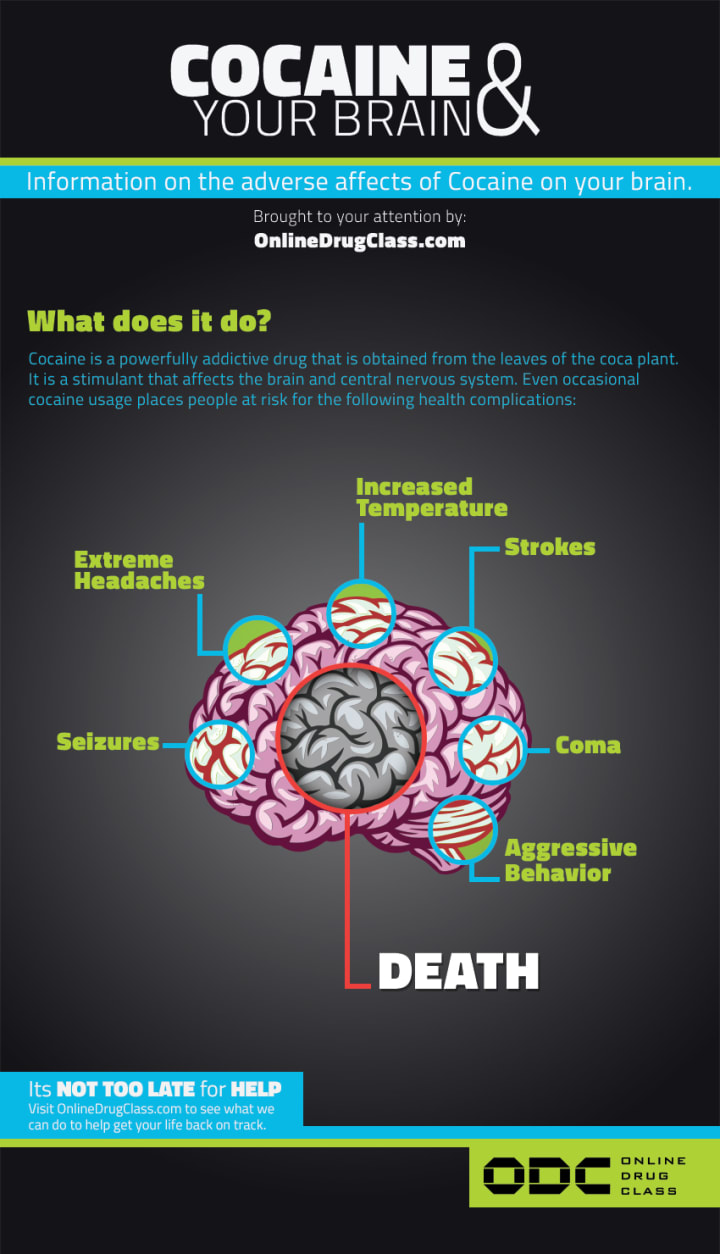
Cocaine works by blocking the reuptake of dopamine, serotonin, and norepinephrine in the brain. By inhibiting the reuptake of dopamine, cocaine increases the concentration of dopamine in the synaptic cleft, leading to prolonged stimulation of dopamine receptors. This results in intense feelings of euphoria, increased energy, and heightened alertness. Similar to amphetamines, the rapid and significant increase in dopamine levels reinforces drug-seeking behavior, contributing to addiction. Chronic use of cocaine can lead to changes in the brain's reward system, including alterations in dopamine receptors and neurotransmitter levels, which further promote addiction and dependence.
Chronic Stress
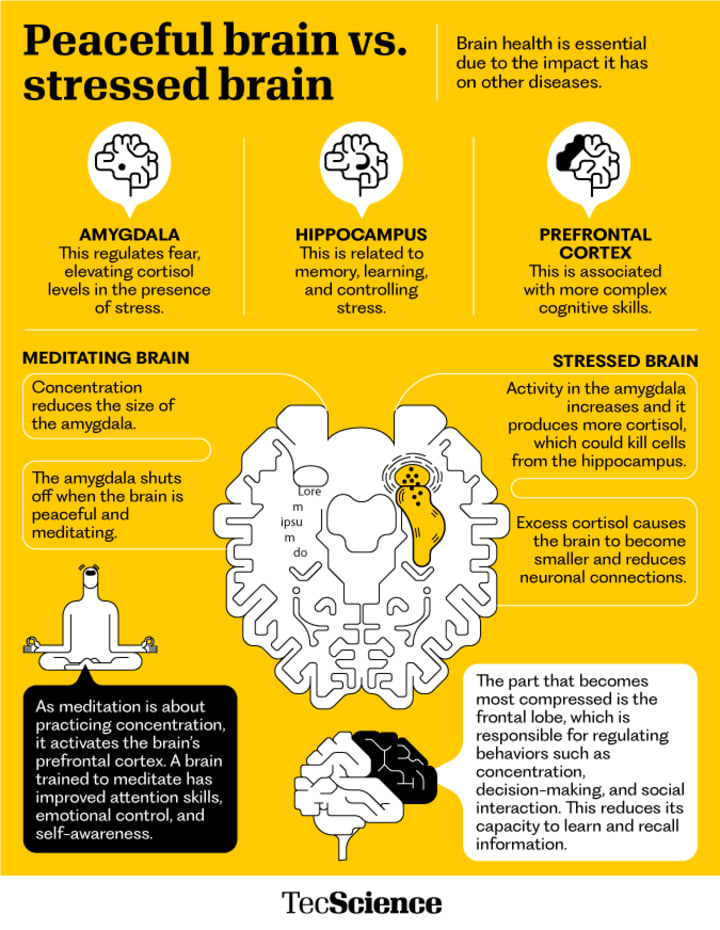
Epinephrine and norepinephrine are like messengers in our body, especially during stressful moments or when we feel excited. They're part of what's called the "fight or flight" reaction, which helps us deal with challenging situations.
When we're stressed or excited, our adrenal glands release epinephrine and norepinephrine into our bloodstream. These chemicals then go to different parts of our body, getting us ready to take action. In our brain, they help us become more alert, focused, and ready to react quickly.
While they don't give us the same feeling of pleasure as dopamine does, epinephrine and norepinephrine can make us feel more energized and attentive. They're like the fuel that gets us ready to handle tough situations.
If we experience a lot of stress over time or keep facing stressful situations (Chronic Stress), it can mess up how our body responds to stress. This can lead to health problems and might even make us more likely to turn to substances like drugs or alcohol to cope with stress. So, while epinephrine and norepinephrine are helpful in the short term, chronic stress can cause problems in the long run.
Desensitization
Desensitization in the brain happens when you get used to something that used to excite you. Let's say you really enjoy playing video games. At first, playing gives you a big thrill and makes you feel good because your brain releases dopamine, which makes you happy.
But if you keep playing video games all the time, your brain starts to get used to it. It's like eating your favorite food every day—it's not as exciting anymore. That's because your brain adjusts by making fewer receptors for dopamine or by becoming less sensitive to it.
So, you need to play more and more to feel the same level of excitement as before. This is called building up a tolerance. It's similar to how you might need to drink more coffee to get the same energy boost if you're used to having it every day.
This desensitization can happen with anything that triggers dopamine release in the brain, like drugs or even certain activities. Over time, your brain gets used to the high levels of dopamine, and you may find it harder to enjoy other things that used to make you happy.
Understanding desensitization helps us see why it's tough to break habits or addictions. It's like your brain gets used to a certain level of excitement, and it takes more and more to feel satisfied. This is why overcoming addiction can be such a challenge—it's not just about willpower; it's also about how your brain responds to the things you do.
Conclusion
In conclusion, addiction to drugs can happen due to a variety of reasons, including genetics and life experiences. Once someone becomes addicted, their brain can be hijacked by the addiction, causing them to lose their control. They become slaves to the addiction, unable to stop even if they want to. Instead of solely punishing those with addiction, it's crucial to offer support like mental health services. Police officers should also receive training to better understand addiction.
By giving people the right support, we can help them break free from addiction and get back to living normal lives. It's important to learn about addiction and its effects so we can help make the world a better place for everyone.
References
https://nida.nih.gov/publications/drugs-brains-behavior-science-addiction/drug-misuse-addiction#:~:text=Addiction%20is%20defined%20as%20a,stress%2C%20and%20self%2Dcontrol.
https://www.samhsa.gov/sites/default/files/programs_campaigns/02._webcast_2_resources.pdf
https://medlineplus.gov/druguseandaddiction.html
https://www.niaaa.nih.gov/publications/cycle-alcohol-addiction
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6352245/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4908125/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6770567/
https://www.samhsa.gov/data/sites/default/files/reports/rpt39443/2021NSDUHFFRRev010323.pdf
Resources for Addiction
SAMHSA National Helpline - 1-800-662-4357 - samhsa.gov/knowtherisks
SAMHSA Center for Substance Abuse Treatment (CSAT) - 866-BUP-CSAT (866-287-2728) - [email protected]
988 Suicide and Crisis Lifeline (Call or Text)
https://www.usa.gov/substance-abuse
https://findtreatment.gov/
https://alcoholtreatment.niaaa.nih.gov/
https://www.samhsa.gov/medications-substance-use-disorders
About the Creator
Amira
Just a writer..songwriting is my specialty! I'm a bit controversial but someone has to fix the narrative..
Enjoyed the story? Support the Creator.
Subscribe for free to receive all their stories in your feed. You could also pledge your support or give them a one-off tip, letting them know you appreciate their work.






Comments
There are no comments for this story
Be the first to respond and start the conversation.