Arthritis or arthritis
Arthritis is very common but not well understood. Actually, "Arthritis" is not a single disease; It is an informal way of referring to joint pain or joint disease. There are over 100 different types of arthritis and related conditions. People of all ages, genders and races can and do have arthritis, and it is the leading cause of disability in America. It is most common in women and occurs more frequently as people get older.
Symptoms of Arthritis
Symptoms come and go. They may be mild, moderate, or severe. They may stay about the same for a few years, but may progress or worsen over time.
Common Arthritis Joint Symptoms – Common Arthritis Joint Symptoms:
Swelling
Pain
Stiffness
Speed limit.
Symptoms of severe arthritis - Severe Arthritis Symptoms:
Severe pain
Inability to perform daily activities
Difficulty walking or climbing stairs.
Permanent joint changes:
(i) These changes may be visible, such as dislocated finger joints, but often the damage can only be seen on X-ray.
Some types of arthritis also affect the heart, eyes, lungs, kidneys, and skin and joints.
Types of arthritis – Different Types of Arthritis
The different types of arthritis are explained below.
Degenerative Arthritis
Osteoarthritis is the most common type of arthritis. When the cartilage -- the slick, cushioning surface on the ends of the bones -- wears away, the bone rubs against the bone, causing pain, swelling and stiffness. Over time, joint strength may decrease and pain may become severe. Risk factors include excess weight, family history, age and previous injury (an anterior cruciate ligament, or ACL, tear, for example).
When osteoarthritis joint symptoms are mild or moderate, they can be controlled by:
Balancing activity with rest
Using hot and cold therapy
Regular physical activity
Maintaining a healthy weight
Strengthening the muscles around the joint for added support
Using assistive devices
Taking over-the-counter (OTC) pain relievers or anti-inflammatory drugs
Avoiding excessive repetitive movements
Inflammatory Arthritis
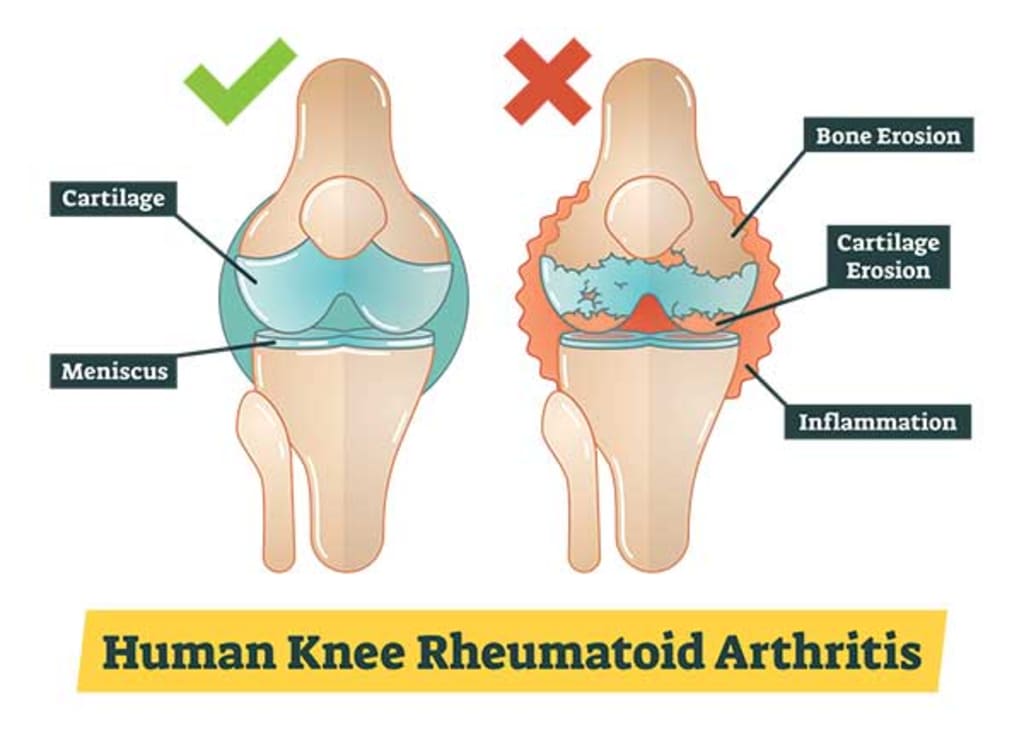
A healthy immune system is protective. It produces internal inflammation to get rid of infection and prevent disease. But the immune system can go haywire, mistakenly attacking the joints with uncontrolled inflammation, which can potentially cause joint erosion and damage to internal organs, the eyes and other parts of the body. Rheumatoid arthritis and psoriatic arthritis are examples of inflammatory arthritis. Researchers believe that a combination of genetics and environmental factors may trigger independence. Smoking is an example of an environmental risk factor that can trigger rheumatoid arthritis in people with certain genes.
With autoimmune and inflammatory types of arthritis, early diagnosis and aggressive treatment are important. Slowing disease activity may help reduce permanent damage. Remission is the goal and may be achieved through the use of one or more drugs called disease modifying antirheumatic drugs (DMARDs). The goals of treatment are to reduce pain, improve function, and prevent further joint damage.
Infectious arthritis
A bacterium, virus or fungus can enter the joint and trigger inflammation. Examples of organisms that can infect joints are salmonella and shigella (food poisoning or contamination), chlamydia and gonorrhea (sexually transmitted diseases) and hepatitis C (blood-to-blood infection, often through shared needles or infection) in many cases. Timely treatment with antibiotics can clear up the joint infection, but sometimes arthritis becomes common.
Metabolic Arthritis
Uric acid is formed as the body breaks down purines, substances found in human cells and in many foods. Some people have high levels of uric acid because they naturally produce more than is needed or the body cannot get rid of uric acid quickly enough. In some people uric acid builds up and forms needle-like crystals in the joints, resulting in sudden spikes of extreme joint pain or a gout attack. Gout can come and go in episodes or, if uric acid levels don't go down, it can become severe, leading to ongoing pain and disability.
Diagnosing Arthritis
Arthritis diagnosis often begins with a primary care physician, who performs a physical exam and may perform blood tests and imaging scans to help determine the type of arthritis. Specialists, or rheumatologists, should be involved if the diagnosis is uncertain or if the arthritis may be inflammatory. Rheumatologists typically manage ongoing treatment for inflammatory arthritis, gout, and other complicated cases. Orthopedic surgeons perform joint surgery, including joint replacement. When arthritis affects other body systems or parts, other specialists, such as an ophthalmologist, dermatologist, or dentist, may also be involved in the health care team.
What can be done about arthritis?
Arthritis is generally plagued by misunderstanding. There are many things that can be done to preserve joint function, mobility, and quality of life. Learning about the disease and treatment options, making time for physical activity, and maintaining a healthy weight are essential.





Comments
There are no comments for this story
Be the first to respond and start the conversation.