True Innovation for Good (Part 1)
A New Zealand-based startup is pioneering foods to improve the quality of care and health outcomes for those with swallowing difficulties. We explore why this nutritional advance is such an important development for those dealing with Alzheimer's and Dementia.

Introduction
More than anything else I have ever written, this article is deeply personal for me. Very personal. When my dad, Barry Wyld, passed this past January from Alzheimer's Disease, he had fought “the good fight” for over a decade. With my mom by his side every step of the way, and through every phase of his mental and physical decline, the health and stress toll on her was considerable. As for myself, I must say that my dad’s long journey into the night has affected me deeply—and changed my perspective on a whole lot of things.
This is the first time I have been moved to write about an innovation in care for those dealing with memory impairment issues and merge my professional expertise with my personal experience as a caregiver. However, this won’t be the last, for as the size, scope and impact of memory care issues unfortunately grows, so to do market opportunities in this area as well.
For those of you who have been fortunate enough to date to not have to deal with a loved one with Alzheimer’s or Dementia, consider yourself truly blessed (and/or "lucky" in the “lotto of life”—so far…). However, with an ever-growing elderly population and the staggering data on what percentage of these individuals who will eventually develop memory-related conditions later in life (and sometimes, way too early), the stark reality is that all too many of us will face dealing with such issues at some point in our lives—either for ourselves or for a family member. If you think the challenges of parenthood are great, they largely pale in comparison to caregiving for a spouse or a parent with memory impairment. And so for those of you with loved ones with memory care issues, my heart goes out to you, for I know the impact of such conditions extends far and deep into the family.
In 2014, my mom finally realized that my father’s decline had reached the point where she could no longer care for him in their home. And so for the last 3+ years of his life, he resided in two different Assisted Living centers in our local area. My Dad’s longevity put him on the far-end of the life expectancy scale for those diagnosed with Alzheimer’s—which we looked upon as both a blessing and a curse (of course, he was always an overachiever!). However, because of his long stay in residential settings, our family did get to meet many families dealing with an aged parent or even a spouse—and in one case a daughter—with early onset Alzheimer’s. Because of the realities of the course of disease progression for those suffering from memory care issues, combined with my Dad’s longevity, my Mom and I saw so many other Alzheimer’s and Dementia patients come and, unfortunately, go during our time.
I say all of this upfront not in hopes of any sympathy. Rather, I state this upfront because, like so many families dealing with loved ones with memory care conditions, you unfortunately become a student of Alzheimer’s and Dementia and a subject matter expert on dealing with the condition and its symptomology. And so when you combine that perspective with my role as a strategic management consultant and professor, I would like to think that I have a unique position to be able to spot what unfortunately are market opportunities when it comes to companies seeking to better serve the ever-growing population of those impacted by these truly debilitating conditions.
And so now, I have my first opportunity to share just such a story with you: that of an innovative company—The Pure Food Co. This New Zealand-based startup is marketing a whole range of foods—and indeed, entire meals—that are prepared specifically to make meal time and digestion easier for anyone who suffers from a health condition that impairs one’s ability to do the fundamental element of the digestive process: that of being able to swallow the food.

Dysphagia Illustrated
My Dad and the "Glob" That No One Wants to See
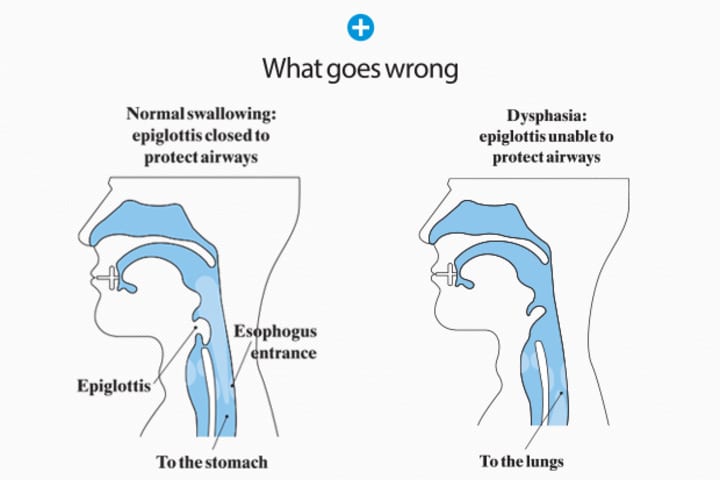
The medical term used to describe difficulty swallowing is Dysphagia. As you can see in the table below, swallowing issues are a more common problem that must be dealt with in dealing with many severe health concerns. Indeed, Dysphagia impacts not just those dealing with Alzheimer’s and Dementia, but in reality, a wide array of diseases—most of which are likewise sadly also chronic in nature.
The A to Z of Eating Difficulties
- Alzheimer's
- Bariatric surgery
- Cerebral palsy
- Cleft lip and palate
- Dysphagia
- Dementia
- Head & Neck Cancer
- Motor Neurone Disease
- Multiple Sclerosis
- Parkinson's Disease
- Stroke
Source: The Pure Food Co (Directory)
What happens in patients with swallowing difficulties
This is where my own personal experience comes in to play in a big way. My dad struggled to eat for the last two years of his life. Early on in his battle with Alzheimer’s, one of the tests that he was put through was what was termed as a “swallow study.” Basically, this is where you are asked to eat jello, munch on a cracker, and drink water while a speech pathologist monitors your chewing and swallowing ability in real time using a form of X-ray called a fluoroscopy.
Now even in the early stages of the disease progression, my Dad was experiencing Dysphagia—hence the testing. However, in the latter stages of his long progression through Alzheimer’s, he experienced extremely severe Dysphagia. Thus, it was a constant battle for him to be able to eat at all, really over the final two years of his life. He was constantly coughing as he ate, and with food, in whatever form it came in, and over time, we had to deal with the ever present threat of aspiration pneumonia, due to food not traveling down his esophagus, but into his lungs.
And based on my family’s simple observations of those caring for those with Alzheimer’s and Dementia, nutrition is key to keeping these folks alive and well. The equation is quite simple—and quite stark: Unless your loved one continues to eat and to drink, they will die. Not eating, or not eating enough to maintain weight, leads to weight loss, lack of energy, and weakness, leading to a whole host of medical complications (including falls and skin conditions), and eventually, death. Not drinking, or not drinking enough to maintain proper hydration, leads to dehydration which can lead to not just bladder issues and kidney problems/failure, but quite commonly, urinary tract infections (UTIs) and other issues as well (on top of the incontinence that is yet another common consequence of the progression of memory care patients that must be dealt with by patients and their caregivers).
For those giving care—both as individual caregivers and for institutions as aides and nurses—for patients with memory issues, the challenges to keeping the person both nourished and hydrated are indeed considerable. This is one of the less talked about, but in reality, most critical aspects of dealing with the progression of Alzheimer's Disease and Dementia. As in my dad’s case, Alzheimer’s patients see a narrowing of their esophagus, physically making it more difficult to swallow. Patients often simply lose their appetites and/or lose the urge to drink. Some patients, like my father, also lose the physical dexterity to simply use table utensils and cups/glasses to be able to feed themselves, making them dependent on others to do so. Only complicating all of this is the loss of social functioning that comes from eating and drinking on one’s own—and the loss of dignity and pride that comes from needing assistance in these crucial activities of daily living (ADLs).
In my own father’s case, he amazingly never lost his appetite, or at least his willingness to eat and drink what was given to him. We would joke within our family, and with his institutional caregivers as well, that he was basically on a “seafood diet,” as he would eat whatever was given to him—and for the last two years he lived, he had to be fed and assisted in his drinking. While being unable to speak, he could express no preference as to what was put in front of him food or drink wise, in whatever form it was delivered—he simply ate and/or drank what was provided. In the institutional environment, patients are routinely tracked and monitored on how much of their meals they ate and what percentage of their liquids they consumed. My dad, again being an overachiever even in his diminished state, consistently “charted” at 100 percent.
However, his eating and drinking so well was not so much a testament to his own perseverance. Rather, it was a testament to the persistence, dedication, and love of both my mom and to his longtime aides. This is because his Dysphagia was so severe that he would routinely cough and momentarily choke on both food and drink. My father only survived because those who fed him, including myself, knew of my dad’s unique ability to eat, cough, choke and then eat again—and likewise to drink, cough, choke and then drink again—often repeatedly during the same meal and/or setting, and were patient enough to diligently work with him to be enable him to almost constantly maintain his weight and only periodically have UTIs. However, what we did and how we did it certainly meant having his aides go far beyond the call of duty and beyond perhaps even what they should have been expected to do in helping him to stay fed and hydrated.
There are ways to help patients cope with the swallowing issues that are at the heart of the inability to eat and/or drink (which may not necessarily decline at the same rate, as it is very patient-specific). The prescribed tactic for assisting patients with difficulty drinking fluids is to add a thickening agent to their water—or any other drink that they might consume. Now this may sound counterintuitive to those unfamiliar with such care, making a liquid thicker actually makes it easier for the patient to swallow. The answer to help those with dealing with Dysphagia, according to all the medical experts, is to switch patients to soft foods and if that doesn’t work, to a puréed diet. Quite often, a puréed diet is turned to as a last resort option for memory care patients and their families/caregivers facing the need to try and maintain proper nutrition in the face of cognitive decline.
My father was taken on and off thickened liquids and switched between "regular" and puréed foods repeatedly during the final two years of his life. Basically, in his unique case, it literally made no difference to him and his ability—or more precisely his inability—to safely eat or drink whether his liquids were thickened or his food was puréed. His eating and drinking was painful, likely both for him and for sure for those who cared for him. And yet, he carried on, and the decision as to whether or not to purée his food was purely made not for his sake, but more so by my mom for her sake. This is because even in the assisted living environment, and with the amount of assistance available to both her and my dad, she insisted on helping him for at least one meal a day—and sometimes, for all three. Admittedly, she had problems dealing with the puréed foods that were provided for him, seeing them as not really suitable for consumption, and without, in his case, helping him to swallow with less effort and difficulty. And so we probably switched back and forth from “regular” foods and a puréed diet a half dozen times in the course of my father’s last two years of life.
What made my mom so resistant to puréed foods for my Dad? It came down to the visual aspect of what he was eating. This was not, however, for lack of trying by the kitchen staff of the two assisted living centers where he lived. In fact, these two facilities actually had food that was well prepared and had taste, which is unusual—some would argue even rare—for the institutional environment. In a regular diet, the food looked appetizing, and the kitchens definitely did everything they could to make the meals as appealing to their residents as human possible. And being in South Louisiana, both facilities even had things like Shrimp Étouffée and Shrimp Po-boys on the menu! Indeed, we were very fortunate to not be in a position to have meals that consisted of anything like a mystery meat and watered-down mashed potatoes, which is the rap on many assisted living centers and nursing homes across the country.
Even when run through the food processor, the meals tasted good overall. However, try as the kitchen staff might, the look and form of food purées for memory care patients take are far, far removed from what you would find on the Food Network site, full of tasty recipes for puréed foods, such as guacamole, hummus, pestos, soups, and desserts. Whether the kitchen puréed foods individually (meaning for a lunch or dinner, my dad’s plate had two, three, or four “globs” on it) or puréed them together (as when the entire meal is combined into one “glob”) was dependent on who might have been on duty and the nature of the meal involved. Yes, the kitchen would often purée something like a Catfish Po-boy or a hamburger into an unrecognizable “glob.”
The fact that I do not have “foodie-type” pictures of some of these delicacies will spare you that imagery, but take what you imagine a puréed cheeseburger, with lettuce, tomatoes, onions, and pickles, put through a food processor and well, it is indeed worse in appearance than you can ever imagine. And so you can imagine, for a patient not as far advanced as was my dad when he was on a puréed diet—and for patients put on puréed foods due to having severe Dysphagia when not having memory issues—the fact that they have to is often a huge obstacle to their recovery and comfort care. Any way you might purée a meal, would you rather eat an actual pork chop or a glob of pork chop for your entree, with sides of green beans and carrots, which bear no resemblance whatsoever—other than their color—to their original state?
Still, the form of the food made no difference to my dad; he saw it and he ate what was fed to him, but it did to my mom, and so she periodically had him switched to “real” food. Either way, he charted consistently eating at “100 percent” - and while it wasn’t pretty and he might have taken two or three times as long as the other patients through both “cajoling” and “comfort” when he experienced swallowing/choking difficulties basically at every meal. Maybe she elected to get him “real food” over the puréed diet much more for herself for having to look at what my dad was eating, but my dad saw and ate it all regardless, to his ever loving credit! However, puréed or unpuréed, my Dad still coughed and choked repeatedly when he ate, so she elected to have him eat “real” food at any opportunity, even speaking to the kitchen staff as to whether or not to purée that night’s dinner or not. Those folks were definitely patient and went above and beyond in dealing not just with my Dad, but with her as his wife and patient advocate as well!
Was there a third way? Was there a way to make puréed foods more palatable—even attractive—to patients like my dad? I wish there had been. However, at the time, there simply was nothing on the market. And still today, there is not a form of puréed foods that is specifically made and marketed for patients dealing with swallowing issues in the United States. However, there is movement toward better solutions for those dealing with Dysphagia, and it is being led by a unique company from way down under—New Zealand, to be specific!
A Look Ahead at the Concluding Part of the Article
In the second part of this article, we will look to the future and see how an exciting development may well bring a better solution to this oft-neglected critical nutrition issue for patients and their caregivers/providers. For those dealing with memory issues and even those suffering with Dysphagia as a secondary condition to the very serious health issue(s) they are dealing with, innovation is finally coming that may make the “glob” that is associated with puréed foods a thing of the past. We will see that this is a global issue and examine exciting innovations from New Zealand—as well as in Europe—that may bring comfort to Alzheimer’s and Dementia patients and those who care for them. And yes, Dysphagia, as unpleasant and chronic as it is, presents a market opportunity that is immense, as these solutions, and likely others, are being developed to cater to this growing, underserved market.

++++++++++++++++++++++++++++++++++++++++++++
Like what you just read? Did it make a difference to you? If so, please see and share this article through social media, email, and even the old-fashioned way of printing it off for a colleague or friend!
And while you’re at it, ask yourself a simple question: Was the info worth a buck or two—or a whole lot more to you, your career, your company? If so, please consider “tipping” (it’s the polite thing to do!) using the easy link below. In providing a small tip, you not only help support the author's work, but you help keep the unique platform that Vocal Media is building be an advertising-free environment - and don't we all need more of that to make our online experiences better today? Please consider showing your support below—and voting for good, ad-free ideas on the Web!
About the Creator
David Wyld
Professor, Consultant, Doer. Founder/Publisher of The IDEA Publishing (http://www.theideapublishing.com/) & Modern Business Press (http://www.modernbusinesspress.com)






Comments
There are no comments for this story
Be the first to respond and start the conversation.