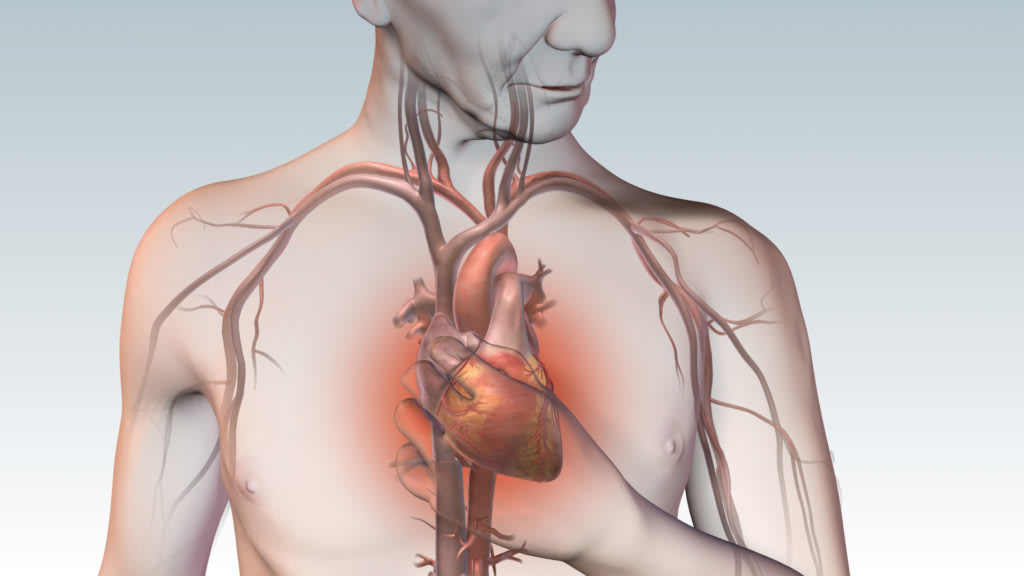
Myocardiodystrophy is a secondary myocardial lesion caused by metabolic disorders and leading to dystrophy and dysfunction of the heart muscle. Myocardiodystrophy is accompanied by cardialgia, cardiac arrhythmias, moderate tachycardia, fatigue, dizziness, shortness of breath. Diagnosis of myocardiodystrophy is based on the data of anamnesis and clinic, electrocardiography, phonocardiography, radiography, echocardiography, MRI, scintigraphy, biochemical blood tests, etc. Treatment of myocardiodystrophy involves pathogenetic therapy with cardiotrophics and symptomatic therapy with antiarrhythmic, antihypertensive drugs, cardiac glycosides, etc.
General information
The term "myocardiodystrophy" (secondary cardiomyopathy, myocardial dystrophy) in cardiology unites a group of non-inflammatory and non-degenerative myocardial lesions accompanied by a pronounced disorder of metabolic processes and a significant decrease in the contractility of the heart muscle. Myocardiodystrophy is always a secondary process involving dysmetabolic, electrolyte, enzyme, neurohumoral and autonomic disorders. Myocardiodystrophy is characterized by dystrophy of myocytes and structures of the conductive system of the heart, which leads to a violation of the main functions of the heart muscle - contractility, excitability, automatism, conduction.
Myocardiodystrophy, especially in its initial stages, is usually reversible, which distinguishes it from degenerative changes of the myocardium that occur with hemochromatosis and amyloidosis of the heart.
Causes of myocardiodystrophy
A variety of external and internal factors that disrupt the flow of metabolism and energy in the myocardium can lead to myocardiodystrophy. Myocardiodystrophy can develop under the influence of:
- acute and chronic exogenous intoxication (alcohol, drug, industrial, etc.), physical agents (radiation, vibration, overheating);
- endocrine and metabolic disorders (thyrotoxicosis, hypothyroidism, hyperparathyroidism, diabetes mellitus, obesity, vitamin deficiency, Cushing's syndrome, pathological menopause);
- systemic diseases (collagenoses, neuromuscular dystrophy),
- infections (chronic tonsillitis, etc.), diseases of the digestive system (liver cirrhosis, pancreatitis, malabsorption syndrome).
The causes of myocardiodystrophy in newborns and young children may be perinatal encephalopathy, intrauterine infections, the syndrome of maladaptation of the cardiovascular system against the background of hypoxia.In athletes, myocardiodystrophy can occur as a result of excessive physical exertion (pathological sports heart).
Pathogenesis
Various adverse factors cause a disorder of electrolyte, protein, and energy metabolism in cardiomyocytes, the accumulation of pathological metabolites. Changes in biochemical processes in the myocardium lead to a violation of the contractile function of muscle fibers, various rhythm and conduction disorders, heart failure. When the etiological factor is eliminated, trophic processes in myocytes can be completely restored. However, with prolonged adverse effects, some cardiomyocytes die and are replaced by connective tissue – cardiosclerosis is formed.
Clinical forms of myocardiodystrophy
Myocardiodystrophy in anemia
Disorders in the myocardium develop with a decrease in hemoglobin to 90-80 g / l. Against this background, hemic hypoxia develops, accompanied by an energy deficit in the myocardium. Anemic myocardiodystrophy can occur with iron deficiency and hemolytic anemia, with acute and chronic blood loss, DIC syndrome.
Clinical manifestations of myocardiodystrophy in anemia are pallor of the skin, dizziness, shortness of breath, tachycardia, increased pulsation of the carotid arteries. Percussion examination reveals the expansion of the boundaries of the heart, indicating myocardial hypertrophy. Auscultation reveals loud heart tones, systolic murmurs over the heart and blood vessels, "top noise" on the cervical vessels. Heart failure develops with prolonged anemia and inadequate treatment.
Myocardiodystrophy in thyrotoxicosis
Under the influence of an excessive amount of thyroid hormones in the heart muscle, the synthesis of adenosine triphosphate (ATP) and creatine phosphate (CF) decreases, which is accompanied by energy, and then protein deficiency. At the same time, thyroid hormones stimulate the activity of the sympathetic nervous system, causing an increase in heart rate, minute blood volume, blood flow rate, BCC. In such conditions, the change in intracardiac hemodynamics cannot be supported energetically, which eventually leads to the development of myocardiodystrophy.
In the clinic of myocardiodystrophy with thyrotoxicosis, arrhythmias (sinus tachycardia, extrasystole, paroxysmal tachycardia, atrial fibrillation) prevail. Prolonged thyrotoxicosis causes chronic circulatory insufficiency, mainly of the right ventricular type, which is manifested by pain in the heart, edema, hepatomegaly. Sometimes thyrotoxicosis is dominated by symptoms of myocardiodystrophy, in connection with which patients turn, first of all, to a cardiologist, and only then get to an endocrinologist.
Myocardiodystrophy in hypothyroidism
The pathogenetic basis of myocardiodystrophy in hypothyroidism is a deficiency of thyroid hormones, leading to a decrease in the activity of metabolism in the myocardium. At the same time, as a result of increased vascular permeability, fluid retention occurs in myocytes, which is accompanied by the development of dysmetabolic and electrolyte disorders (an increase in sodium content and a decrease in potassium).
Myocardiodystrophy in hypothyroidism is characterized by constant aching pains in the heart, arrhythmias (sinus bradycardia), blockades (atrial, atrioventricular, ventricular).
Alcoholic and toxic myocardiodystrophy
It is believed that the daily intake of 80-100 ml of ethyl alcohol for 10 years leads to alcoholic myocardiodystrophy. However, with a hereditary deficiency of a number of enzymes that break down ethanol, stress, frequent viral infections, myocardiodystrophy can develop in a shorter time – in 2-3 years, even with the use of smaller amounts of alcohol. Alcoholic myocardiodystrophy occurs mainly in men 20-50 years old.
Toxic myocardiodystrophy occurs in people receiving long-term therapy with immunosuppressants (cytostatics, glucocorticosteroids), NSAIDs, some antibiotics, tranquilizers, as well as poisoning with chloroform, phosphorus, arsenic, carbon monoxide, etc. Such variants of myocardiodystrophy can occur in cardialgic (painful), acute arrhythmic, combined and stagnant forms.
The cardialgic form of myocardiodystrophy is characterized by aching or aching pains in the chest, a transient sensation of heat or chilliness of the extremities, sweating. Patients are concerned about general weakness, fatigue, decreased physical endurance, headaches.
The arrhythmic form of myocardiodystrophy is accompanied by tachycardia, disturbances of the rhythm and conduction of the heart (sinus tachycardia or bradycardia, extrasystole, blockades of the legs of the Gis bundle), sometimes - attacks of fibrillation and atrial flutter. With a combined form of myocardiodystrophy, arrhythmias and cardialgias are noted. Manifestations of congestive myocardiodystrophy are caused by heart failure and include shortness of breath under stress, cough, attacks of cardiac asthma, swelling on the legs, hydropericardium, hydrothorax, hepatomegaly, ascites.
Tonsillogenic myocardiodystrophy
Myocardial lesions with tonsillitis occur in 30-60% of patients. Tonsillogenic myocardiodystrophy usually develops after a series of angina, occurring with high fever and intoxication. In the clinic of tonsillogenic myocardiodystrophy, complaints of intense pain in the heart area, pronounced weakness, irregular pulse, shortness of breath, focal or diffuse sweating, subfebrility, arthralgia prevail.
Myocardiodystrophy of physical overstrain
Develops in athletes performing physical activities that exceed their individual capabilities. In this case, hidden chronic foci of infection in the body can contribute to myocardial damage - sinusitis, tonsillitis, adnexitis, etc.; lack of proper rest between workouts, etc. A number of theories have been put forward regarding the pathogenesis of myocardiodystrophy of physical tension: hypoxic, neurodystrophic, steroid-electrolyte.
This variant of myocardiodystrophy is mainly manifested by symptoms of a general nature: weakness, lethargy, fatigue, depressed mood, decreased interest in sports. There may be palpitations, tingling in the heart area, interruptions.
Menopausal myocardiodystrophy
It develops as a result of dishormonal processes in women aged 45-50 years. Menopausal myocardiodystrophy is manifested by pain in the heart area of a pressing, stabbing or aching nature, radiating into the left arm. Cardialgia increases due to "hot flashes", accompanied by a feeling of heat, palpitations, increased sweating. Heart failure in menopausal myocardiodystrophy may develop with concomitant hypertension.
Diagnosis of myocardiodystrophy
Patients with a history of myocardiodystrophy usually have diseases or pathological conditions accompanied by tissue hypoxic syndrome and impaired metabolic processes. An objective examination of the heart reveals an irregular pulse, muffling of heart tones, weakening of the I tone at the apex, systolic noise.
Electrocardiography records various arrhythmias, violations of the processes of myocardial repolarization, a decrease in the contractile function of the myocardium. Carrying out stress and pharmacological tests for myocardiodystrophy, as a rule, gives negative results. Phonocardiography detects changes in the ratio of the duration of electrical and mechanical systole, the appearance of a gallop rhythm and systolic noise at the base and apex, muffling of heart tones. Echocardiography determines the expansion of the chambers of the heart, changes in the structure of the myocardium, and the absence of organic pathology.
The myopathic configuration of the heart detected by chest radiography indicates a deep myocardial lesion. Scintigraphy makes it possible to assess the metabolism and perfusion of the myocardium, to identify focal and diffuse defects of accumulation as indicating a decrease in the number of functioning cardiomyocytes.
A biopsy of the heart muscle is resorted to in doubtful cases, when non-invasive studies are uninformative. The differential diagnosis of myocardiodystrophy is carried out with coronary heart disease, myocarditis, atherosclerotic cardiosclerosis, pulmonary heart disease, heart defects.
Treatment of myocardiodystrophy
Complex therapy of myocardiodystrophy consists of the treatment of the underlying disease, pathogenetic (metabolic) and symptomatic therapy. In this regard, the therapeutic tactics for myocardiodystrophy is determined not only by a cardiologist, but also by narrow specialists - a hematologist, an otolaryngologist, an endocrinologist, a rheumatologist, an endocrinologist gynecologist, a sports doctor. Patients are recommended a gentle physical regime, the exclusion of harmful professional influences, contact with chemicals, alcohol intake and smoking.
Metabolic therapy of myocardiodystrophy involves the appointment of B vitamins, cocarboxylase, ATP, potassium and magnesium preparations, inosine, anabolic steroids and other drugs that improve metabolic processes and nutrition of the heart muscle.
In case of heart failure, diuretics, cardiac glycosides are indicated; in case of arrhythmias, antiarrhythmic agents are indicated. In menopausal myocardiodystrophy, HRT, sedative and hypotensive drugs are prescribed. Etiotropic therapy of tonsillogenic myocardiodystrophy requires intensive treatment of tonsillitis up to tonsillectomy.
Prognosis and prevention of myocardiodystrophy
The reversibility of myocardial changes in myocardiodystrophy depends on the timeliness and adequacy of treatment of the underlying disease. The outcome of long-term myocardiodystrophy is myocardiosclerosis and heart failure.
Prevention of myocardiodystrophy is based on the elimination of current diseases, taking into account age and physical fitness when playing sports, abstaining from alcohol, eliminating occupational hazards, proper nutrition, mandatory rehabilitation of foci of infection. Repeated drug courses of cardiotrophic therapy 2-3 times a year are recommended.
About the Creator
Artur Kh.
Writer, doctor and businessman. I blog about self-development, personal growth, health and new ways of making money.





Comments
There are no comments for this story
Be the first to respond and start the conversation.