Pennsylvania State University researchers have added a new one to the studies in the field of cancer research.
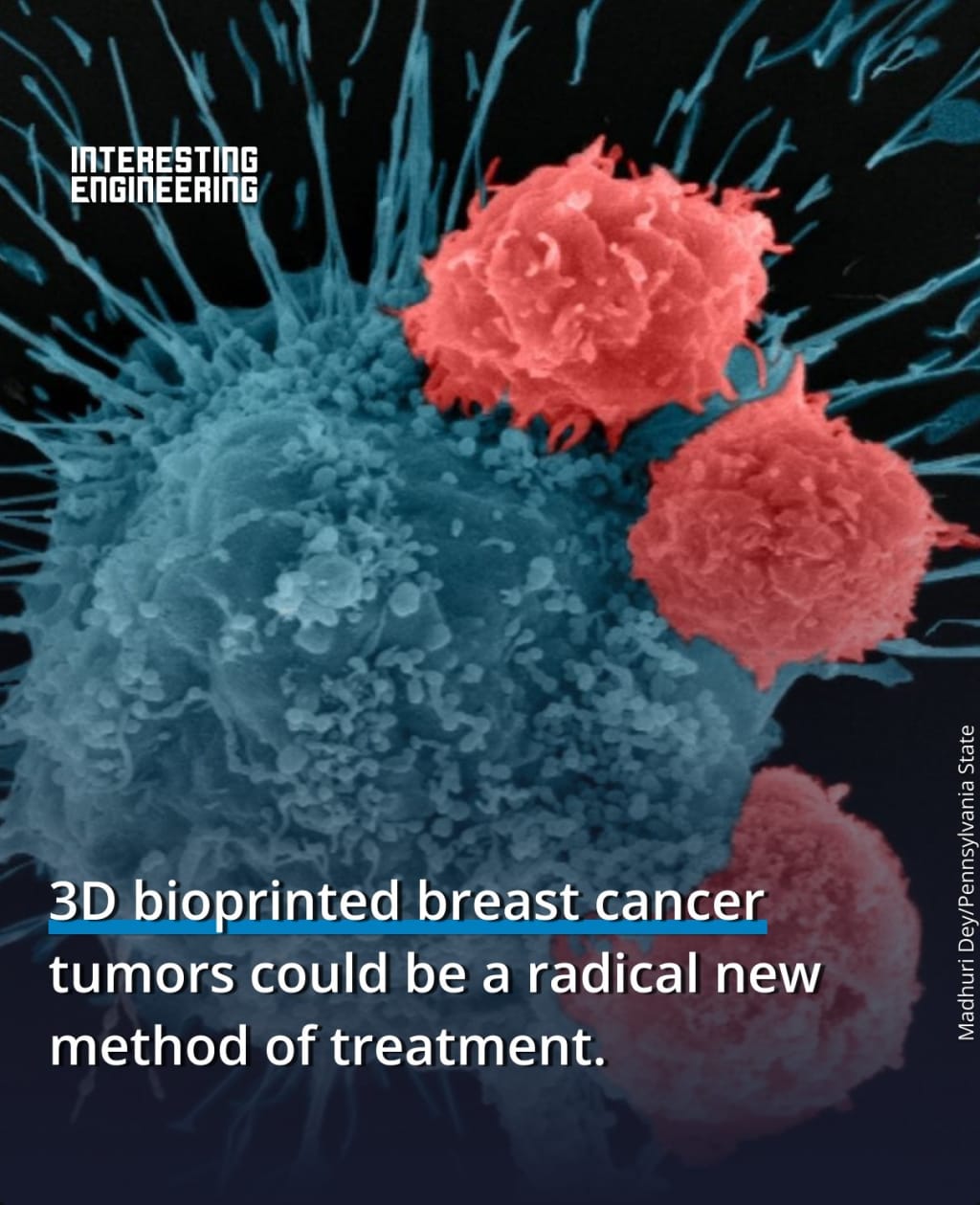
In a new study on comprehending a condition that is one of the main causes of mortality worldwide, researchers 3D bioprinted breast cancer tumors and treated them.
According to studies carried out in the Ozbolat lab, the accomplishment establishes the framework for precisely fabricating tumor models. The invention will make it possible to research and create anticancer treatments in the future without using "in vivo" (in animal) testing.
“This will help us understand how human immune cells interact with solid tumors,” said Ibrahim Ozbolat, professor of engineering science and mechanics, biomedical engineering, and neurosurgery at Penn State and the senior author of the study.
“We’ve developed a tool that serves as a clinical test platform to safely and accurately evaluate experimental therapies. It is also a research platform for immunologists and biologists to understand how the tumor grows, how it interacts with human cells, and how it metastasizes and spreads in the body.”
A New Technique
To precisely pinpoint tumors in three dimensions and produce the tissue, the researchers employed aspiration-assisted bioprinting, a relatively recent technique.
After creating a multi-scale vascularized breast tumor model out of the tissue, the researchers found that chemotherapy and cell-based immunotherapeutics had an effect on the tumor.
The scientists employed doxorubicin, a chemotherapeutic medication based on an anthracycline that is frequently used to treat breast cancer, to first validate the accuracy of its tumor model.
The researchers worked with Dr. Derya Unutmaz, an immunologist at Jackson Laboratory, to evaluate a cell-based immunotherapeutic treatment on the tumor after discovering the bioprinted tumor reacted to chemotherapy.
They used human CAR-T cells
Human CAR-T cells that had been modified through gene editing were employed by the researchers to identify and combat an aggressive subtype of breast cancer cells.
The researchers discovered that the cells within the bioprinted tumor had triggered a favorable immune response and were warding off the cancer cells after 72 hours of the modified CAR-T cells being circulated within the tumor.
“Our model is made from human cells, but what we make is a very simplified version of the human body,” Ozbolat said.
“There are many details that exist in the native microenvironment that we aren’t able to replicate, or even consider replicating. We are aiming for simplicity within complexity. We want to have a fundamental understanding of how these systems work — and we need the growth process to be streamlined because we don’t have time to wait for tumors to grow at their natural pace.”
Ozbolat and his colleagues are now working with tumors removed from actual breast cancer patients.
The research is also supported by The National Cancer Institute, the National Science Foundation, and the H.G. Barsumian, M.D. Memorial Fund, and TUBITAK.
The articles were published in Advanced Functional Materials and Biofabrication on October 3.
Abstract:
Despite substantial advancements in development of cancer treatments, lack of standardized and physiologically-relevant in vitro testing platforms limit the early screening of anticancer agents. A major barrier is the complex interplay between the tumor microenvironment and immune response. To tackle this, a dynamic-flow based 3D bioprinted multi-scale vascularized breast tumor model, responding to chemo and immunotherapeutics is developed. Heterotypic tumors are precisely bioprinted at pre-defined distances from a perfused vasculature, exhibit tumor angiogenesis and cancer cell invasion into the perfused vasculature. Bioprinted tumors treated with varying dosages of doxorubicin for 72 h portray a dose-dependent drug response behavior. More importantly, a cell based immune therapy approach is explored by perfusing HER2-targeting chimeric antigen receptor (CAR) modified CD8+ T cells for 24 or 72 h. Extensive CAR-T cell recruitment to the endothelium, substantial T cell activation and infiltration to the tumor site, resulted in up to ≈70% reduction in tumor volumes. The presented platform paves the way for a robust, precisely fabricated, and physiologically-relevant tumor model for future translation of anti-cancer therapies to personalized medicine.






Comments
There are no comments for this story
Be the first to respond and start the conversation.