What If There’s Not “A Place for Mom?” As America Faces a Looming Nursing Home Crisis
With an acute labor shortage and increased operating costs, a significant percentage of skilled nursing facilities in the U.S. are functioning at a loss. Recent research shows that many of these nursing homes face shutting down if nothing changes. We look at what this will mean for health care - and for all of us - moving forward.

Introduction
So, you think that you have a tough management job? Well, as challenging as it might be, it’s likely far, far easier than being a nursing home administrator these days. Now no doubt, managing a nursing home was hard prior to 2020. But throw in COVID and a crazy labor market, and today, there is likely no greater challenge out there in the world of organizations, for-profit, non-profit, or public sector, than to be in charge of a skilled nursing facility - the formal name for what are commonly referred to by lay and medical people alike as “nursing homes” - today.
Nursing homes. Now, we don’t even like to think about them for the most part. Many don’t like to - or even won’t - set foot inside of one, even if they have a beloved grandparent or parent in a skilled nursing facility. And certainly, one of almost everyone’s life goals is to not end up as a patient in a nursing home.
And yes, they are tough - extremely tough - places to work! To say that working in a nursing home is not like working at Google or a tech startup - or even a nice restaurant or warehouse - is putting it mildly. You deal with difficult conditions, difficult situations, and yes, difficult people. And yes, you have to deal with the grim reality of nursing homes. This is the fact that when you have a large number of mostly elderly people under one roof, many of whom have serious, often multiple, physically and mentally debilitating conditions, and your patients pass away - often. Nursing homes have relied for decades on an army of low-paid aides, some who have a CNA (Certified Nursing Assistant) designation while others, where allowed by state law, are just those willing to work in such a facility for low pay. All of this makes for a highly stressed working environment, and as a result, nursing homes always face high turnover, even in “normal” economic and non-pandemic conditions, across all of their staff. And of course, as nursing homes are tough places to work, they are just as tough to manage in an effective manner.
Today, this is more true than ever. And a recent report from the AHCA (American Health Care Association) shows just how hard it is to staff a nursing home today and just how serious the staffing situation is at present. In fact, the worker shortage is causing major operational and financial problems across the nursing home industry in the United States, problems that are not just limiting care, but also posing very real existential threats to a considerable portion of skilled nursing facilities across the country! And so in this article, we will dive into the ACHA’s data and provide some practical and policy suggestions for addressing what is a nursing home staffing crisis today that could easily - quite easily and rapidly in fact - morph into a nursing home crisis very, very soon for all of us in the U.S.

A Staffing Crisis That is Fast Becoming an Even Larger Crisis for the Nursing Home Industry
This Spring, the AHCA conducted a major survey of over 700 nursing home administrators on the state of their businesses - and the results were, to put it mildly, alarming. The trade group published its findings earlier this month (June 2022) in its report, State of the Nursing Home Industry. In it, the AHCA researchers showed just how serious staffing issues are across almost all skilled nursing facilities in the U.S.. They went on to show how a shortage of workers is impacting not just nursing homes' abilities to provide patient care today, but is threatening their very viability to remain in business, even in the near term.
Let’s take a look at the major findings from the AHCA’s study. First, nursing homes are facing an acute - and worsening - staffing situation today. As can be seen in Figure 1 (Nursing Home Administrators’ Opinions of Their Current Staffing Situations), the vast majority of skilled nursing facility administrators surveyed presently report having a very real - and acute - shortage of staff. In fact, only 2% - yes, 2% - of nursing homes today are fully staffed, while an additional 11% are having “minor” (low level) staffing shortages, The remaining 87% - yes, almost 9 in 10 skilled nursing facilities - are currently experiencing either moderate (39%) or high level (48%) shortages of personnel. And as Figure 2 (Nursing Home Administrators’ Opinions of Their Staffing Situation, May vs. January 2022) shows, those in charge of the nation’s skilled nursing facilities feel
Figure 1: Nursing Home Administrators’ Opinions of Their Current Staffing Situations
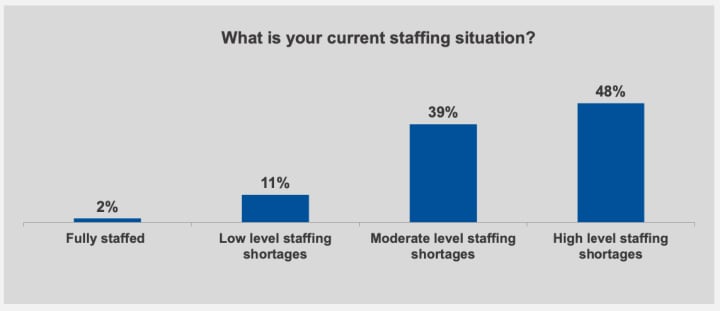
Source: American Health Care Association, State of the Nursing Home Industry, June 2022 (Used with permission)
that their staffing woes are, in fact, only getting worse, with a third of respondents believing that their workforce situation has gotten much worse thus far in 2022, and another 27% sensing that it has become somewhat worse.
Figure 2: Nursing Home Administrators’ Opinions of Their Staffing Situation, May vs. January 2022
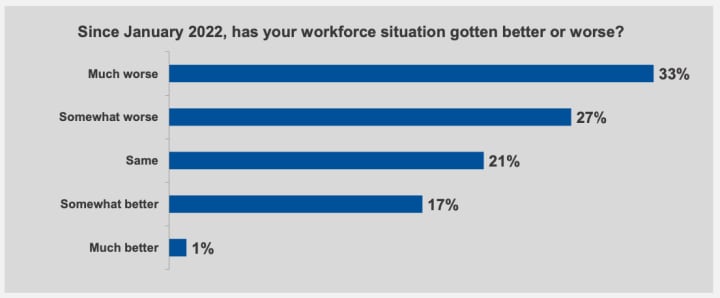
Source: American Health Care Association, State of the Nursing Home Industry, June 2022 (Used with permission)
Now, nursing home administrators report that they have at least attempted to be quite proactive in their efforts to counter the worker shortage that they are currently experiencing. As can be seen below in Figure 3 (Nursing Home Administrators’ Strategies to Deal with Their Present Staffing Shortages), those in charge of the nation’s skilled nursing facilities have undertaken a number of initiatives - often multiple and interlinked - to try to not just incentive the hiring of new staff, but to better retain the staff that they have what is today an increasingly competitive job market, especially for front-line service workers. All of these tactics in some way involve “throwing money at the problem,” as not just increasing wages (95%), offering bonuses (92%), and/or promoting workers faster (68%) adds to the total personnel costs for a nursing home. Offering workers more paid training and educational opportunities (71%) and more efforts to improve the workplace culture (i.e. through team building activities, “fun” incentives, etc.) cost money to a facility as well. All of these strategies to better be able to recruit and retain employees only adds to the operating costs of a skilled nursing facility, which worsens their financial outlooks, both individually and collectively (more on that in a few minutes).
Figure 3: Nursing Home Administrators’ Strategies to Deal with Their Present Staffing Shortages
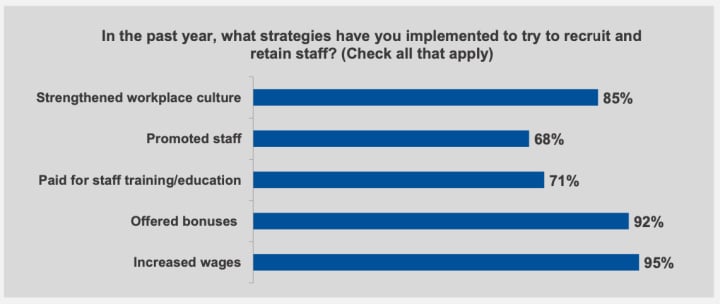
Source: American Health Care Association, State of the Nursing Home Industry, June 2022 (Used with permission)
Now, hiring employees willing to work in a skilled nursing facility has, yes, always been a challenging proposition. Front-line nursing home caregivers are, by and large, young and female. Many have children of their own for which they are responsible. Many also come from disadvantaged backgrounds, and many deal with serious challenges in their own lives, economically, living conditions, relationships and familial concerns, etc. As such, many of the people who are the “best prospects” for serving in these front-line roles face serious obstacles to even working outside of the home at all. As can be seen in Figure 4 (Nursing Home Administrators' Recognition of the Obstacles Involved in Hiring Staff) below, nursing home administrators are struggling to find willing - and able - workers to staff their patient care and support positions, as the vast majority report having difficulty not just attracting interested, qualified candidates for these roles. They also say that they recognize that one of the chief reasons that there indeed are a lack of qualified candidates to work in their skilled nursing facilities is that the vast majority of those who could work in these roles have personal commitments that prevent them from working outside of their home at all! As such, these are intransigent, structural, societal-level issues (i.e. child care, the social safety net, health care, addiction, and more) that are beyond the control of any one nursing home or the entire skilled nursing industry, but that do need to be dealt with by policymakers at the federal and state levels.
Figure 4: Nursing Home Administrators' Recognition of the Obstacles Involved in Hiring Staff
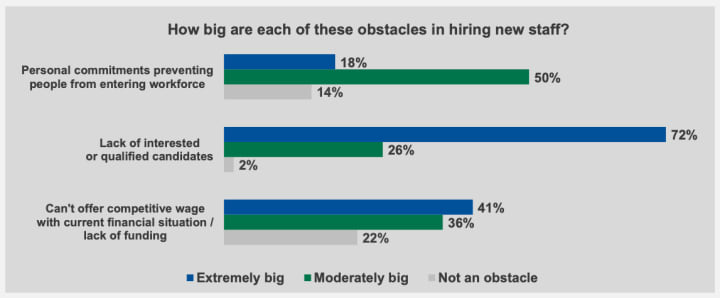
Source: American Health Care Association, State of the Nursing Home Industry, June 2022 (Used with permission)
And so at present, here in mid-2022, skilled nursing facilities are experiencing a very real staffing shortage that administrators are finding tough to resolve and which is having a very real impact not just on patient care, but on the financial viability of their operations. As one would expect from the foregoing survey results, nursing home administrators today are reporting that they are having an extremely difficult time hiring new personnel to help alleviate their present staffing crisis. In fact, as can be seen in Figure 5 (Nursing Home Administrators' Difficulty in Hiring New Staff Today [May 2022]) below, fully 98% of skilled nursing facility administrators report that it is presently very (58%) or moderately (40%) difficult to hire new staff, with only a scant 2% saying that it was a somewhat easy task - and 0% - no one - out of the over 700 administrators surveyed by the AHCA saying that it was “very easy” to hire new workers right now!
Figure 5: Nursing Home Administrators' Difficulty in Hiring New Staff Today (May 2022)
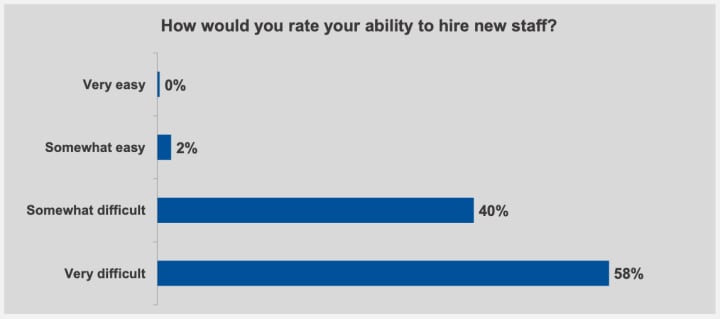
Source: American Health Care Association, State of the Nursing Home Industry, June 2022 (Used with permission)
The present staffing shortage is indeed translating into both serious patient care and financial problems for nursing homes across the country. As one can see in Figure 6 (Nursing Home Administrators' Actions Taken in Response to Staffing Shortages), 61% of skilled nursing facility administrators are reporting that they are having to limit new patient admissions at their nursing homes. Additionally, even with the reduced number of patients that they can care for at their facilities, 71% of these administrators are having to hire temporary agency staff (who are far more expensive to have working at a facility than having their own caregiving workers) to cover the patient workload and yes, 99% are asking (read as making) their present employees to work overtime. All of this contributes to increased overhead costs for these facilities, and when combined with a diminished patient load (which yes, means diminished revenues), one can easily see how the financial outlook for nursing homes is not good at present - and may only deteriorate in the future. According to the AHCA’s
Figure 6: Nursing Home Administrators' Actions Taken in Response to Staffing Shortages
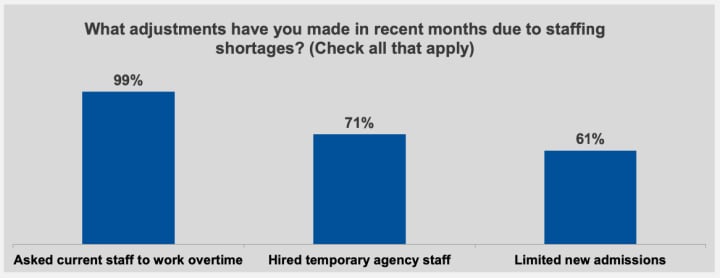
Source: American Health Care Association, State of the Nursing Home Industry, June 2022 (Used with permission)
research, nursing home administrators reported that their operating costs have soared by - on average - 41% year-over-year, and that the largest chunk of these increased costs come from rising wages and other measures undertaken by them to combat the staffing shortage. As you can see in Figures 7 (Nursing Home Administrators' Reporting on Their Current Operating Situation) and 8 (Nursing Home Administrators' Concerns About Keeping Their Own Facility Operating) , these rising costs, combined with shrinking patient loads, are combining to cause a bleak outlook for skilled nursing facilities going forward. As Figure 7 shows, almost 6 in 10 nursing homes are today operating at a loss, with just over a third of all skilled nursing facilities operating at a margin of less than 3%.
Figure 7: Nursing Home Administrators' Reporting on Their Current Operating Situation
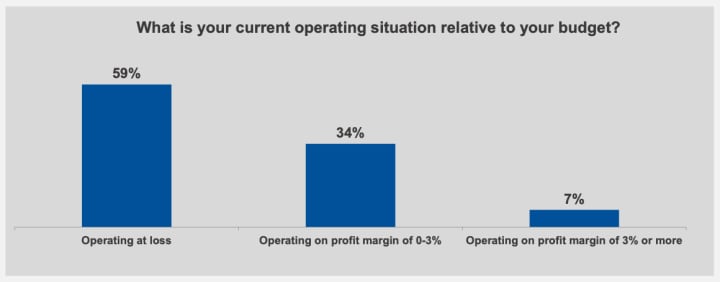
Source: American Health Care Association, State of the Nursing Home Industry, June 2022 (Used with permission)
And as can be seen in Figure 8, the combination of rising costs and decreased revenue is concerning nursing home administrators. In fact, almost three quarters of these administrators see the workforce shortages as a threat to their own facility’s ability to financially and operationally survive! In fact, as Figure 9 (Nursing Home Administrators’ Beliefs About
Figure 8: Nursing Home Administrators’ Concerns About Keeping Their Own Facility Operating
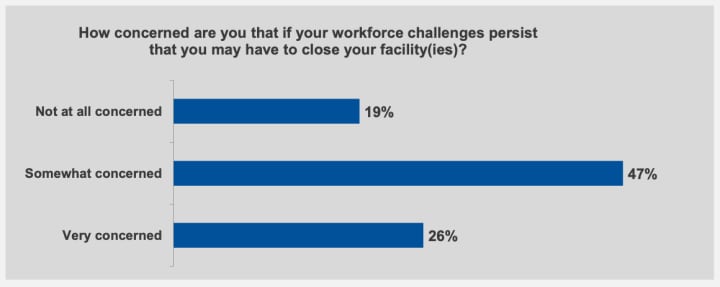
Source: American Health Care Association, State of the Nursing Home Industry, June 2022 (Used with permission)
How Long Their Own Facility Can Operate At Its Current Pace) shows, more than half of nursing home administrators do not believe that they can operate their facilities at their current pace for more than one year.
Figure 9: Nursing Home Administrators’ Beliefs About How Long Their Own Facility Can Operate At Its Current Pace
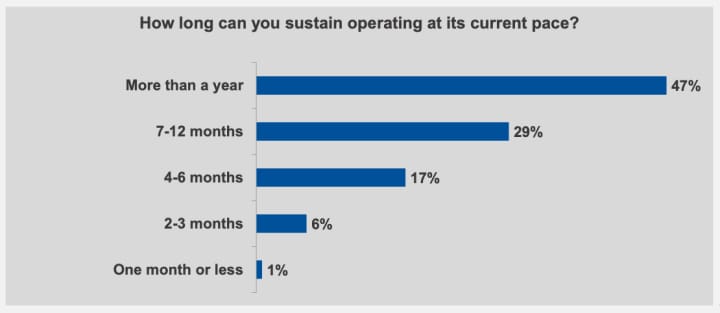
Source: American Health Care Association, State of the Nursing Home Industry, June 2022 (Used with permission)
And yes, nursing home administrators are right to be concerned about the potential for the current staffing shortage - and resulting operational and financial difficulties for nursing home operators - to be nothing less than existential threats to their facilities and their jobs - and the jobs of their employees. According to a separate report from the AHCA, produced in coordination with the NCAL (National Center for Assisted Living), 2022 looks to be a record year - by far - for nursing home closures, as more than 400 facilities are predicted to close in the coming year (See Figure 10: Nursing Home Closures, 2015-2022). And of course, when a nursing home has to close, the impacts are far ranging, as such closures impact not just those employed at the facility, but the current patients and their families - and in a wider sense, the health of the community by eliminating a needed outpost for care for seniors and more.
Figure 10: Nursing Home Closures, 2015-2022
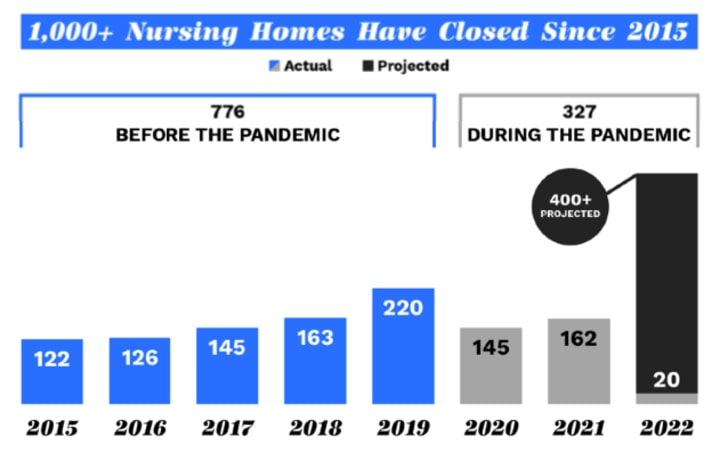
Source: American Health Care Association, Nursing Home Closures: By the Numbers, June 2022 (Used with permission)
Analysis
In the end, all of this should be quite concerning not just for those employed in the long-term care industry, but in truth, for all of us! According to the latest data from the CDC/National Center for Health Statistics, America’s nursing homes have well in excess of 1 million residents. And with not just the financial and operational difficulties facing skilled nursing facilities all across the country today, but proposed changes in Medicare reimbursements and other federal funding, approximately a third of all nursing homes are at risk of closure and thus, their patients are facing potential displacement. So there could indeed be a great disruption facing the nursing home industry over the next year or more, one that necessitates serious consideration from federal and state policymakers. As Mark Parkinson, President and CEO of AHCA/NCAL, put it bluntly recently:
“Every (nursing home) closure is like a family being broken apart, with the lives of residents, staff and their families impacted in the process. With hundreds of nursing home closures looming now and thousands more anticipated if government funding is cut, state and federal policymakers need to step up to support our social safety net. We need to do better than just keep nursing home doors open—we need to make significant investments to better support our frontline caregivers and transform facilities for a growing elderly population.”
As a strategic management consultant and professor (and yes, one who has had his elderly mother in a skilled nursing facility), I can say that there are no easy answers to what is fast becoming a nursing home crisis, not simply a staffing crisis. In sum, we, as a society, have come to depend on having “a place for Mom (and/or Dad).” However, with the staffing and financial woes whipsawing the nursing home industry today, we could well not be able to depend on skilled nursing care being as readily available as it is today in your respective locale. All of this will necessitate not just innovative practices in the industry, but serious political debate on how such necessary long-term care can and should be provided over the long-term.

++++++++++++++++++++++++++++++++++++++++++++++++++++
About David Wyld
David Wyld is a Professor of Strategic Management at Southeastern Louisiana University in Hammond, Louisiana. He is a management consultant, researcher/writer, publisher, executive educator, and experienced expert witness. You can view all of his work at https://authory.com/DavidWyld.
Social Media Links to David Wyld:
About the Creator
David Wyld
Professor, Consultant, Doer. Founder/Publisher of The IDEA Publishing (http://www.theideapublishing.com/) & Modern Business Press (http://www.modernbusinesspress.com)






Comments
There are no comments for this story
Be the first to respond and start the conversation.