Emergency Preparedness Experiences by Emergency Managers
Rural Hospitals of the Pacific Northwest - Chapter 2: Literature Review Dr.Gabriella Kőrösi
Introduction
The purpose of this qualitative research study was to increase the understanding of the new EP rule and its implications for rural hospital preparedness in the Pacific Northwest, including identification of common themes emerging amongst health care facility EP personal. Regulations from the Federal government require hospitals to prepare for disasters (Levinson, 2014). Review of current literature was essential to understand the impact of EP in rural hospitals and communities. The identified themes helped to recognize potential barriers, create supportive recommendations for health care facilities, including hospitals, that are undergoing the implementation and maintenance process of the EP rule. Emergency and disasters can be underestimated in scale (Cirkovic, Sandberg, & Bostrom, 2010). For example, Landman et al. (2015) described the responses and lessons learned at the Brigham and Women's Hospital in Boston after the Boston Marathon bombing. Findings included needed improvement in workflow, patient naming conventions, information systems, situational awareness, documentation, orders and procedures. The resilience of communities and EP staff, especially in hospitals, is a crucial element for survival during and after a disaster (Charney et al., 2014). There are many articles regarding disasters and EP of hospitals and hospital staff after disasters, including quantitative and qualitative inquires. Currently there is a gap in the literature regarding the EP in Pacific Northwest rural coastal communities (Savoia et al., 2017; Paganini et al., 2016; Alim et al., 2015; Hammad et al., 2017; Woods, 2016; Fagbuyi et al., 2016; Seale, 2010; Shipman et al., 2016; Palttala et al., 2012). In the literature I found common themes related to EP that will be discussed later in the review. The influencers of EP included hospital preparedness, preparedness of hospital staff, the role of a preparedness coordinator, relevant staff training and education, responsiveness to disasters and communication needs during a disaster (Savoia et al., 2017; Paganini et al., 2016; Alim et al., 2015; Hammad et al., 2017; Woods, 2016; Fagbuyi et al., 2016; Seale, 2010; Shipman et al., 2016; Palttala et al., 2012). Gaps in the current literature have been identified and will be discussed below. Chapter 2 includes an introduction, literature search strategy, a more detailed theoretical framework discussion, a detailed literature review and a conclusion.
Literature Search Strategy
To locate current relevant literature, multiple databases were searched: CINAHL and MEDLINE combined, MEDLINE with full text, Thoreau, ProQuest Central, Walden University dissertations, Walden University Health Sciences and related research, Embase, ScienceDirect, Sage journals, PubMed, Academic Research Complete and Google. Search terms used in the literature review included emergency preparedness, Federal Emergency Management Agency, disaster response, humanitarian response, disaster response mental health, competencies disaster mental health, hazard response, emergency management, natural disasters, emergency response, communication, role of communication, risk communication, hospital preparedness, disaster preparedness, healthcare system, phenomenology, narrative inquiry, CMS EP rule, earthquakes, Cascadia subduction zone, earthquakes in Pacific Northwest, mass casualty disasters, protection of research participants, and complexity theory framework. Only current and relevant literature were chosen to be included in the literature review.
Theoretical Considerations - Complexity Theory and Framework
Complexity theory emerges from complex systems and complex thinking (Reed, Howe, Doyle, & Bell, 2018). Complexity theory looks at individual parts of any system and how they work together (Thrift, 1999; Thomson et al., 2016). The theory works with multiple level systems, addresses the complexity of interactions of systems, its parts; unpredictability within these systems; works for community health systems, institutions and organizations like hospitals (Hilhorst, 2003; Paley & Eva, 2011; Thrift, 1999; Thomson et al., 2016; Reed et al., 2018; Long, McDermott, & Meadows, 2018; Brand, Fleming, & Wyatt, 2015). Complexity in the context of disaster and risks related to disaster fits well as disasters and emergencies do not have boundaries, changing in scale and response need, and a disaster in one area of the world can affect other people in other regions (Hilhorst, 2003; Long et al., 2018; VanVactor, 2016). Similar to complexity theory and complex systems thinking EP is complex requires multiple individuals and systems to work together, interact and adapt to what is happening around them and come up with creative solutions in disasters (Byng & Jones, 2004; Plsek & Greenhalgh, 2001; Reed et al., 2018; Long et al., 2018). Local conditions in an emergency can create a very powerful emergent effect, just like in complexity theory the effects would depend on how all parts add together to create a system behavior (Byng & Jones, 2004; Thomson et al., 2016; Brand et al., 2015). A complex system can be unpredictable in its behavior just like disasters and emergencies, like earthquakes, depending on the situations that arise (Comfort, 1995; Hilhorst, 2003; Plsek & Greenhalgh, 2001; Reed et al., 2018; Long et al., 2018; Brand et al., 2015; Brand et al., 2015). Thomson et al., (2016) describes complexity as a characteristic of a system that looks at relationships and behaviors of a system, how the parts work together and the interactions between the individual parts of the system. Long et al., (2018) describes complexity theory as complex adaptive systems in a health services research with multiple elements including embeddedness, unclear boundaries, distributed control around the system, unpredictability coupled with a nonlinear relation, changes that occur in any scale can change the reaction of the system and adaptability. Reed et al. (2018) describes the importance of complex systems thinking in understanding the experiences people have working well together with the planned research of EP managers and their experiences. Complexity theory asserts that the individual parts of the system work separately but form a response together that creates a system behavior or reaction and this reaction is based on the exchange of information between individuals (Thomson et al., 2016; Reed et al., 2018; Brand et al., 2015). Complexity theory fits the EP system as the system has multiple parts that work separately but form a response together to a disaster or emergency (Thomson et al., 2016; Reed et al., 2018). VanVactor (2016) describes a disaster response as a complex and dynamic environment where there is changes and uncertainty prevails. Each response to a disaster will be different, thus the interacting parts remain changing continuously (VanVactor, 2016). Complexity theory is being used more frequently in health sciences in qualitative studies (Thomson et al., 2016; Long et al., 2018). Reed et al (2018) had developed a SHIFT -evidence framework based on complexity theory in healthcare systems including three strategic principles with 12 simple rules (Reed et al., 2018):
1. Act scientifically and pragmatically
· Understand problems and opportunities,
· Identify, test and iteratively develop potential, solutions,
· Assess whether improvement is achieved, and capture and share learning,
· Invest in continual improvement
2. Embrace complexity
· Understand processes and practices of care
· Understand the types and sources of variation
· Identify systemic issues
· Seek political, strategic and financial alignment
3. Engage and empower
· Actively engage those responsible for and affected by change
· Facilitate dialogue
· Foster a culture of willingness to learn and freedom to act
· Provide headroom, resources, training and support

Figure 1. SHIFT - Evidence conceptual framework. (Reed et al., 2018).
Long et al. (2018) discusses that complexity theory does not attempt to control the research but looks at all the parts that interact, identify patterns and how that affect the system as a whole. Based on the description above I believe that Complexity theory and the adaptation of the SHIFT evidence framework based on the theory would be a good fit for this qualitative research to look at EP in the hospital setting and how the preparedness rule implementation effects the Pacific Northwest community.
Structure and Influencers of Hospital Preparedness
Markiewicz et al. (2010) conducted qualitative study using interviews to understand EP and epidemiologist support between hospitals and public health department in North Carolina. Methods included surveys and semi-structured interviews. Coding and analysis were done using ATLAS.ti program. Quantitative descriptive statistics were analyzed with Microsoft Excel program. The study results have found a positive effect on communication, disease surveillance; EP and response with an epidemiologist present (Markiewicz et al., 2010). The study recommends similar programs in other communities for EP indicating a potential solution for communication between hospitals and public health is having an epidemiologist on staff (Markiewicz et al., 2010). Levinson (2014) surveyed 174 hospitals and conducted 10 site visits, additionally he interviewed state hospital associations and health care coalitions in the Connecticut, New Jersey and New York area. Of 173 hospitals 153, 89% reported having difficulty during Hurricane Sandy, including problems with patient care and staffing (Levinson, 2014). Additionally, problems were identified with infrastructure, including electrical and communication problems and difficulties with community collaboration over resources, transportation and fuel (Levinson, 2014). Rahm and Reddick (2011) explored Chief Administrative Officers (CAO) and their risk perceptions related to disasters and emergencies. The study used surveys from US cities. A total of 131 surveys collected with 76.5% response rate (Rahm & Reddick 2011). The study was evaluated using contingency table analysis and it was found that CAO's have misinterpretations of the threat to their cities; some think that their city is more vulnerable than other cities; some think the threat is not as much as in other cities when this is not the case (Rahm & Reddick 2011). The study suggests the need for future studies exploring CAO's actions taken for disaster preparedness based on their perception of risk (Rahm & Reddick, 2011).
Hospital Preparedness
Mellow, Bloch and Grimes (2018), Ramsey Hamilton and Miller (2017) and Elko (2017) describes hospital preparedness framework according to the CMS Rule including four major elements: a. Risk assessment of local hazards prior to creating a plan and planning for emergencies once the assessment is completed. b. Developing policies and procedures for emergencies that align with the risk assessment, policies and procedures must have an annual review. c. Providing communication plan according to state and federal laws, sharing information and carrying out safe patient care locally as well as state wide, if needed, timely and effectively. d. Providing adequate training with yearly review and testing for EP with hospital and community drills to practice preparedness.
Taschner, Nannini, Laccetti and Greene (2017) examined EP policy and practice in Massachusetts hospitals after 9/11/2001 using a qualitative inquiry. The case study used purposeful sampling and a snowball method. Data collection included key informant interviews and review of policies, programs, and directives. Research findings included emerging themes: standardized training needs, importance of communication and collaboration, effects of funding creating financial burden for hospitals (Taschner et al. 2017). This study showed the need for future research and identified funding and training needs for hospitals with new EP rules and policies that require implementation. Cagliuso (2012, 2014, 2014a) also used a qualitative phenomenological study to explore the EP in hospitals and stakeholders' views on preparedness. The method uses a phenomenological approach with stakeholders in Middle Atlantic state metropolitan area; using semi - structured in depth interviews based on a developed interview protocol. The study confirms the need for future research based on the themes found, that supports the planned qualitative inquiry in EP in health care settings. The study had a developed interview protocol. The outcome included stakeholders finding the system positive, effective, time consuming and ineffective. The study found emerging themes of necessity for funding, essential elements included collaboration, communication, coordination; in role of the government the study participants had mixed views and the need for hospital leadership buy in for success was identified (Cagliuso, 2014a). Cagliuso (2014a) concludes that future studies are needed for additional support in EP.
Christian, Kollek and Schwartz (2005) described hospital preparedness in Canada as having appropriate planning for the facilities, training for the staff, appropriate equipment and planned exercises. Although EP should be current all the time, Christian, Kollek and Schwartz (2005) found that disaster plans in hospitals are only checked every few years for accreditation purposes. The authors recommend exercises for disasters to be done at least once a year (Christian, Kollek, & Schwartz, 2005). Liu et al. (2018) found that hospitals could benefit from increasing collaboration with outside agencies for disaster preparedness. Currently many hospitals prepare and communicate internally or maybe with some governmental agencies but do not include additional community partners in the planning process (Liu et al. 2018). Levinson (2014) found that 47 hospitals had difficulty with communication during Hurricane Sandy. Additionally, collaboration outside of the hospitals created challenges (Levinson, 2014). Increasing outer agency collaboration and practicing full scale disaster drill exercises could be very beneficial for EP (Liu et al., 2018). Hospitals were used as shelters during the Hurricane, that created additional difficulties including the use of limited resources for people who did not have a medical need (Levinson, 2014).
Looking at two hospitals in Texas Dallas Woods (2016) found that collaboration with external governmental agencies like the Centers for Disease Control and Prevention (CDC) are vital to successfully manage Ebola and prevent the spread of the disease. The study revealed the importance of hospitals keeping up to date on new protocols, training staff to prevent disease spread and correct diagnosis (Woods, 2016). In these cases, Emory University hospital was up to date with its protocol and was able to manage patients well while Texas Health was not prepared, and that gap of knowledge and lack of protocol led to misdiagnosis, spreading of the disease and deaths (Woods, 2016).
Joint commission
Elko (2018) described the new requirements added by the Joint Commission's survey on performance of the 2016 CMS EP Rule. Requirements include: steadiness of operations and succession plans; documentation of partnership with local, tribal, regional, state, and federal EM officials (Elko, 2018). Additional requirements include: upkeep of contact information on volunteers including tribal groups', continuous training of new and existing staff, including any contractors and volunteers; annual trainings; integrated health care systems and transplant hospitals (Elko, 2018). Levinson (2014) found that most of the hospitals, 157 out of 171, that had difficulty during the response for Hurricane Sandy had received citations before from hospital surveyors. Collaboration at the community level, as well as State and Federal level, is recommended during major disasters (Levinson, 2014).
Disaster Planning and Logistics
VanVactor (2016) used a qualitative, quasi - case study approach to improve understanding of the processes related emergency planning, logistics and evaluate the interaction between emergency management, disaster planning and the United States Department of Defense (US DoD). The author discussed the need for flexibility during disasters, breaking down silos between organizations, the importance of collaboration between agencies, stakeholders and building community resilience (VanVactor, 2016). Participants included n=20 military leaders (VanVactor, 2016). Difficulties in logistics include the complex nature of a disaster that even during the disaster there is information that is not known that can lead into disruption on the supply chains (VanVactor, 2016). VanVactor (2016) recommends that professionals whom work in the supply - chain need to have built relationships and practice to function more seamlessly during a disaster. Additionally, increased understanding through scientific research before, during and after disasters can also increase effectiveness of efforts in preparedness, response and resilience for disasters (VanVactor, 2016). Obaid et al. (2017) observed that failure to appropriate planning for disasters including infrastructure development can cause patient deaths and legal consequences. Additional planning problems included lack of staff knowledge and lack of coordination in the region (Obaid et al. 2017).
Preparedness
Egli (2013 & 2014) discussed the results of her exploratory study on EP in the United States using interviews, policy review and case studies. The goal of the study was to find opportunities for better preparedness, resilience and response (Egli, 2013; Egli, 2014). Egli (2013 & 2014) and Sobelson, Wigington, Harp and Bronson (2015) asserts that collaborative thinking and resilience building is essential to EP in all levels of community and government. Resilience and preparedness investment are beneficial as each dollar spent now saves 4 dollars in the future (Egli, 2013; Egli 2014). Preparedness includes the need for stable infrastructure (Egli, 2013; Egli, 2014; Obaid et al. 2017). Currently there is only a low 2% of the US GDP is spent on infrastructure maintenance that can include highways, bridges, water supply (Egli, 2013; Egli, 2014). There is a great emphasis on individual preparedness recommended by FEMA as a first step for disasters where a person should be able to self-sustain for at least 72 hours (Egli, 2013; Egli, 2014; Sobelson et al. 2015). VanVactor (2016) and Obaid et al. (2017) described that a well-prepared community is knowledgeable of the incident command system (ICS), know how to take care people in mass casualty incidents, have the knowledge and ability for risk reduction and prioritizing needs. Looking at previous disasters for preparedness is essential and the military has a well-tested action review tool developed in 1993 that uses four points and three questions that helps identify readiness for a disaster, response to a disaster and ability to respond (VanVactor, 2016, p.171).
Community approach
Sobelson et al. (2015) conducted informal conversations with n=88 stakeholders regarding emergency management in the community and preformed a qualitative analysis by using deductive codes. The authors used a literature review and environmental scan to identify the 7 programs in the communities using a whole community approach in EP (Sobelson et al. 2015). The authors used conference calls, site visits, workshops and final reports to collect their data (Sobelson et al. 2015). Findings included leadership experienced in previous disaster and recovery, leadership is visionary, and realist and these attributes help with a successful start of a program and community engagement (Sobelson et al. 2015). Additional findings included for successful preparedness relationship building, community events for engagement, recruitment and recognition of staff and volunteers, preparedness partners can include anyone from the community, the preparedness is culturally appropriate and simple (Sobelson et al., 2015). Sobelson et al. (2015) concluded that a more detailed guidance is needed for a whole community approach to support communities with the analytical tools needed for preparedness. Future research suggested for measurements of community resiliency (Sobelson et al. 2015).
Vulnerable populations
Fagbuyi et al. (2016) discussed medical countermeasures (MCM) for children in public health emergencies. The American Academy of Pediatrics disaster preparedness advisory council had looked at gaps remaining for children in disasters (Fagbuyi et al. 2016). Difficulties arise from medications, antitoxins, medical devices, lifesaving equipment's and vaccinations, that are lack in supply, or approved for adults but not children, national stockpiles not prepared enough, to address the need of children, whom are almost one fourth of the US population (Fagbuyi et al. 2016). Recommendations from the American Academy of Pediatrics include increased research support, emergency access to medications that are not approved, improving distribution plan and increasing pediatric stockpiles of MCM, pediatric preparedness prioritization, informing pediatric providers on current and up to date use of MCM's and their distribution plan in case of an emergency (Fagbuyi et al. 2016). McDermott, Martin and Gardner (2016) reviewed disaster response needs for people with disabilities. Essential elements for successful disaster response include collaboration at local, state and national level, knowing people with resources, the depth of resources available and building relationships at all levels of private and governmental sectors (McDermott et al. 2016). Math, Nirmala, Moirangthem and Kumar (2015) reviewed articles from 1978- 2013 to define, classify and discuss disasters from the mental health point of view. Math et al., (2015) stated that in a disaster people with mental health issues are 2–3 times higher than in the population whom are not experiencing a disaster. Mental health responses to disaster can include but not limited to relapse to prior mental health disorders, guilt, grief, fear, mental illness, relapse or new substance use, suicidal ideas, death wish, (Math et al. 2015). Abnormal grief reactions that require trauma and grief focused treatment can persist in over 70% of earthquake survivors (Math et al. 2015). Common mental health disorders in a disaster struck population include adjustment disorders, post-traumatic stress disorders (PTSD) anxiety, depression disorders and substance abuse are some examples (Math et al. 2015; North & Pfefferbaum, 2013). Recommendations included avoid mental health labeling to prevent stigmatization, training the public to be able to provide simple community-based interventions like groups, art therapy, yoga, mediation; instead of only medical professionals providing care (Math et al. 2015). North and Pfefferbaum (2013) conducted a literature search and review n mental health interventions and service delivery in disasters. Findings included the need for integration of mental health services into disaster response, need for providing accurate mental health assessments in a disaster setting, and after the disaster when PTSD and other psychiatric symptoms are most likely develop (North & Pfefferbaum, 2013).
Hospital Staff Preparedness
The research by Shipman et al. (2016) looked nurses whom were first responders in a disaster and in a setting of a shelter or a temporary medical clinic. The study used the phenomenological approach narrative inquiry to identify themes on the participant's reflections (Shipman et al. 2016). Shipman et al. (2016) interviewed 10 nurses about their experiences, used 15 open-ended questions. Themes identified based on the interview questions include: the role of the nurse, knowing the plan and growth, the experience (Shipman et al. 2016). The role of the nurse also had subthemes including: organization, physical assessment, psychosocial needs, and resourcefulness (Shipman et al. 2016). Shipman et al. (2016) found that previous exercise in mass casualty training did not help the nurses to prepare for the disaster in a community setting. Shipman et al. (2016) highlights the need to teach nursing students about community responses in case on a disaster. The 172 hospitals involved during Hurricane Sandy all had at least one community wide disaster preparedness response event in the prior year and still experienced multiple difficulties during the storm (Levinson, 2014).
Seale (2010) in the narrative description after Hurricanes Rita and Ike found that additional staff preparation and planning is needed for successful EP. The purpose of the study was to provide disaster preparedness improvement in based on experiences from two Hurricanes in a postacute rehabilitation facility. The methods included a narrative description of the evacuation events of Hurricane Rita and Hurricane Ike. The outcomes show that additional disaster preparedness is required beyond the licensing requirements for EP to be successful in a disaster. The author recommends developing a contingency plan, staff preparation, exploring creativity for evacuation and transportation. The study showed one way to describe a qualitative inquiry by using a narrative to describe the previous events that happened and what had been learned. The planned EP study will have parts that could be described as a narrative including documents in the facilities that describe the EP plan. This article highlights previous gaps in preparedness and support needed for future EP implementation.
Hodge, Miller and Dilts Skaggs (2017) in their quantitative study used a survey to look at EP for nurses and have found nurses had difficulties with EP terms and activities, ethical issues, and access to resources. The study was a quantitative survey that was sent out to nurses via e-mail. Data was analyzed using multiple logistic regression and descriptive statistics. Outcomes in the study found problems in areas of preparedness terms and activities, ethical issues, and access to resources. Based on the study a plan for additional education was developed. The study shows the emergency disaster preparedness needs and conflicts from a nursing perspective in a rural hospital setting. This study outlined the need for additional support and education for nurses in a rural hospital to prepare for disasters.
In a Saudi Arabian study by Alzahrani and Kyratsis (2017) looked at nursing preparedness in hospitals, the authors have found training variances, including the lack of awareness and knowledge of emergency disaster preparedness plans among nurses. The authors examined nurses' knowledge, skills, and awareness of emergency disaster response during mass gatherings. The study design was cross sectional online survey, among four hospital's nursing staff in Saudi Arabia, Mecca (Alzahrani & Kyratsis 2017). A non-probability purposeful sampling was used in the study (Alzahrani & Kyratsis 2017). SPSS was used to get data for descriptive statistics, including mean, median, mode, frequencies, percentages, SD, cross tabulation. The need was identified for communication outreach, education, and skill development (Alzahrani & Kyratsis 2017). This quantitative study showed the need between consistent EP training and education need in hospital EP.
Charney, Rebmann and Flood (2014) conducted a survey of hospital personnel after a tornado in Missouri. Response rate of 23.4% with n= 1234 healthcare workers, the researchers used SPSS for data analysis. Data analysis included multivariate logistic regression, linear regression, McNemar tests, Chi squared, descriptive statistics, additionally the good model fit, and t-tests (Charney et al. 2014). Prior preparedness was a great indicator for future willingness to work in a disaster (Charney et al. 2014). Staff who participated working after the tornado showed more willingness to work again in a disaster (Charney et al. 2014). Childcare was found an obstacle to go to work, 61% of staff had childcare needs during the week after the tornado, and 54% used alternative childcare (Charney et al. 2014). Of the respondents 51% stated they would have used childcare if it was offered by the hospital, increasing the likelihood for reporting to work (Charney et al. 2014). Baack and Alfred (2013) conducted a study to identify rural nurse's readiness in Texas for disasters. The study was a descriptive correlational design and used surveys that were answered by N = 620 nurses. Statistical analysis included priori power analysis for multiple regression. The study found that nurses did not feel that they are prepared for a disaster response. The authors suggest that additional training for nurses in disaster preparedness is indicated, to ensure appropriate safe response to an occurring disaster. Veenema et al. (2016) explored nurse's role in disaster preparedness and response. The authors underline the importance of nurses' role in disaster response as nursing is the largest medical workforce in the United States. The project come up with recommendation for nurses in policy, training, education and research for disaster response. The authors call for a coordinated approach to provide appropriate education that has previously been not provided.
Public Health Departments
Gossip et al. (2017) conducted a rapid realist review of 44 articles and explored monitoring, and evaluation of the disaster response; including the lack of improvement on effectiveness in public health departments. Gossip et al. (2017) asserts that monitoring and evaluation in disaster response is a critical part to improve future disaster responses. Findings included current struggles for health departments to learn from prior mistakes, the need standardized forms used in disaster response, positive leadership in local health departments, increase learning and training opportunities as well as collaboration with community partners including sharing information related to disaster responses. To improve disaster response and strengthen the local department functions identification of currents risks, strengths of the departments, areas where improvements are needed, including updating policies and procedures is needed (Gossip et al. 2017). Shah, Newell and Whitworth (2016) studied local health departments and their capability related to EP and informatics. The study used Poisson regression analysis from the 2013 National Profile of Local Health Departments (LHD) survey n= 505 subsample was selected to be included in this analysis (Shah, 2016). The results had found that 38.3% of the local health departments participated in exercises or drills in the previous 12 months to prepare for emergencies. The researchers additionally found that writing and developing an emergency plan was 86.9%among LCH's, preparedness training for staff was 84.3% and tabletop exercises were 76.4%, assessment of staff preparedness 66% (Shah, 2016). LCD's with higher informatics capabilities had more EP activities than other LHD's (Shah, 2016). Shah (2016) discussed the importance of EP exercises as a need for real life events and the concern that only a small portion of LHD's participated in full scale exercises in the last 12 months.
EP Coordinator
Goss (2017) in the qualitative inquiry looked at the risk perceptions of all hazard pandemic emergency planning in a Red River Emergency Operation Center in North Texas. Goss (2017) used semi structured interviews with the EP managers. Hand coding and thematic analysis was used for data interpretation (Goss, 2017). Themes identified from the study included political climate, emergency response, training, experience and communication (Goss, 2017). Findings of the study included lack of effective communication and coordination, lack of trust in government, and shortfalls in training (Goss, 2017). Adini, Laor and Aharonson (2014) in their study looked at hospital preparedness in Israel for pandemic influenza, found essential factors that influence preparedness. Israel developed a national policy, and hospitals developed standard operating procedures (SOP), for pandemic influenza (Adini et al. 2014). The authors conducted a quasi - experimental study, used surveys that were sent out twice to hospital managers to evaluate pandemic preparedness (Adini et al. 2014). Results conducted by looking for correlations with logistic regression analysis (Adini et al. 2014). Findings included the benefits of SOP, developed based on guidelines from the Ministry of Health (MOH), knowledge about the disease, and preparedness evaluation (Adini et al. 2014). Shah (2016) found that having an EP coordinator at the local health department increased preparedness activities by 1.28 times. Bennett, Phillips and Davis (2017) looked emergency managers and their role in integrating techniques like wireless technology that help disaster response and recovery focusing on people with disabilities and benefiting the whole community. The authors found that incorporation of wireless technologies can help at the individual household level as well as during preparation and recovery in disasters (Bennett et al. 2017).
Education and Training
Shipman et al. (2016) believed that there is not enough community EP thought in nursing schools. All the authors were professors in nursing, or education, based on their titles and description in the article (Shipman et al. 2016). Based on that and the need for further education in the article the authors have a strong belief in the importance of education and preparing new nurses for disaster response (Shipman et al. 2016). The description and telling the story of the lived experiences of first-time nurses who responded to disasters, proved the gap in the nursing education on EP (Shipman et al., 2016). Liu, Fowler, Roberts and Herovic (2018) in their qualitative inquiry found that additional training and education needed for nurses, relating crises communication, and ethical decision making, during an emergency related to a disaster. During emergencies nurses might have to make decisions, regarding patient care that would be outside the law, and their comfort zone (Liu et al. 2018). Alim, Kawabata and Nakazawa (2015) looked at disaster preparedness training and drills for nursing students. The authors used nursing students in their study and created an 8 hour one-day training in disaster preparedness training and drill n =225 (Alim et al. 2015). The study evaluated how well the training worked by a 20 question pre and posttest, observation of study participants during the drill using a Likert scale and interviews n=40 randomly chosen participants (Alim et al. 2015). Alim et al. (2015) used R 3.0.0 for statistical analysis using paired t-tests. The total of n= 309 students participated in the training, the researchers found that the students' knowledge significantly improved in the post test compared to the pre-disaster training test (Alim et al. 2015). The interview results in 73% of the cases indicated that students understood what need to be done in a disaster (Alim et al. 2015). The authors have concluded that additional studies and disaster training curriculum needed to evaluate the success of disaster training for nursing students (Alim et al. 2015).
Paganini et al. (2016) looked at EP in Italian hospitals using interviews in qualitative study. The researchers found that emergency room physicians have a lack of knowledge, on what to do during a disaster; because of this finding education and training needs were identified. The study was cross sectional design with a convenience sample. The researchers conducted structured interviews. Data was analyzed by frequencies for respondent characteristics, by Mann - Whitney test for non-parametric data, and the Kruskal -Wallis test. The results identified lack in knowledge, of EP in a disaster, by the physicians on duty. Italy has a policy for hospital preparedness that need to be followed like the EP rule in the US. The study found inadequate disaster preparedness in the hospital's ED department (Paganini et al. 2016). This finding is an indication of a potential gap between EP rule and implementation (Paganini et al. 2016). The Israeli study by Adini et al. (2014) suggests that hospital managers who have knowledge about different emergency scenarios, have increased capacity and preparedness to respond to an emergency. Practicing drills did not seemed to be effective, for pandemic purposes, but the authors acknowledge that it is beneficial for mass casualty incidents (Adini et al. 2014). Gap in knowledge was found regarding personal protective equipment for staff in case of a pandemic, authors suggest the cause was ineffective communication to staff (Adini et al. 2014).
Wallace (2016) explored the development of a peer support pilot project for emergency responders, to provide encouragement and emotional support if the need arises. The goal of the project was to increase operational effectiveness, and increase resilience of personnel (Wallace, 2016). During deployment in a disaster there is multiple trauma, and emotional impact, experienced by the disaster relief personnel, related to witnessing destruction to property and human suffering (Wallace, 2016). Wallace (2016) found the peer support model effective in the pilot project. This implicates that potential trainings in other settlings, like hospitals, and community disaster response systems, could be useful to provide emotional support for staff during a disaster. Obaid et al., (2017) developed EP training for rural communities and analyzed findings after training. Rural communities have less resources and resources are more dispersed causing difficulties to respond to a disaster (Obaid et al. 2017). The exercise was a three-hour long training and a three-hour conference after the training with n= 83 command center participation (Obaid et al. 2017). The participants were evaluated based on their emergency operation plan adherence and intra agency coordination (Obaid et al. 2017). Findings included problems with communication, not knowing how to request additional staff and assets for support, not using the Incident Command system, not knowing who to contact for transfers not having the incident action plans (Obaid et al. 2017). Obaid et al. (2017) recommended the use of disaster exercises for disaster planning to assess and practice multi agency and organization practice before a disaster. Ripoll et al. (2015) conducted a systematic literature review, to identify competencies for disaster management, and response to develop competency-based education. The study used the systematic reviews and meta-analysis checklist and included scholarly papers between 2004 -2014 using 38 articles after exclusion criteria (Ripoll et al. 2015). The authors asserted that education needs to be based on a well-defined core set of competencies to build the required knowledge and skills for disaster preparedness and response (Ripoll et al. 2015). Findings included the lack in consistent terminology use, the need for standardizing disaster preparedness and response education that is multi-disciplinary (Ripoll et al. 2015). Current findings included that most disaster preparedness studies are focusing on health care and the nursing response (Ripoll et al. 2015).
Standards of care
Leider, DeBruin, Reynolds, Koch and Seaberg (2017) in their literature review explored ethical guidance offered as part of crisis standards of care (CSC) in disaster response. He researchers reviewed relevant literature and found some controversy about standards of care during a disaster (Leider et al. 2017). Issues arise between individual provider responsibility versus a systemic response to a disaster and liability for the standards of care provided (Leider et al. 2017). The authors recommend prior planning from federal to local level to provide the best possible care during a disaster (Leider et al. 2017). Additionally, prior planning can support providers following treating people in the most ethically and legally appropriate way even in less than desirable circumstances like a mass causality incident (Leider et al. 2017). VanVactor (2016) described the main goal of supply chain support during the disaster is to help health care professionals decrease the risks associated with health needs during the disaster.
Responsiveness to Emergencies During a Disaster
Responding to a disaster needs knowledgeable and well-trained professionals, the job is highly stressful, for any personnel in disaster preparedness (Wallace, 2016). Ablah et al. (2010) used surveys across 23 states, with n =522 responses, to explore the collaboration between community health centers, and local health departments. Surveys were sent by e-mail, based on available directory of health departments, and community health centers (Ablah et al. 2010). The survey included four different themes related to disaster preparedness: demographics information, collaborative disaster preparedness and disaster response and disaster plan knowledge (Ablah et al. 2010). Data analysis software SPSS was used to look at frequencies, t-test and chi-square (Ablah et al. 2010). The study found that while there is collaboration between community health centers and local health departments, there is a lack of exercises of EP drills that are practical (Ablah et al. 2010). Reporting on the response to Haiti's earthquake in 2010 Martin, Nolte and Vitolo (2016) explored the disaster response between international disaster relief agencies, by looking at the four C's: collaboration, communication, coordination and cooperation. The researchers used the e-mail communications, and 8 face to face interviews between organizations, to analyze the four C's (Martin et al. 2016). The e-mails represented 47 individuals from different organizations, the data included 150 pages (Martin et al. 2016). Results indicated that 15% of the e-mails related to communication, cooperation pointed to courtesy and respect between the organizations (Martin et al. 2016). Coordination appeared to be a one-way announcement, in many cases, where organizations announced what is their plan (Martin et al. 2016). Collaboration was found difficult to find, in the e-mails, the researchers suspect it was related to new organizations arrived at the scene in Haiti every day (Martin et al. 2016).
Catalino (2015) in his qualitative inquiry looked at vulnerable populations in a disaster response, status post Hurricane Katrina, and the impact of the Federal Legislation. Catalino (2015) interviewed 5 emergency managers in Louisiana, he used open ended interview questions. The study used snowball sampling method and thematic analysis (Catalino, 2015). Catalino (2015) found 15 emerging themes that included: increased coordination between state and federal agencies, increased planning efforts, regional coordination, increased storm preparedness. Challenges included language barriers, lack of funding, transportation difficulties, not enough sheltering and providing for people whom are sick and not able to move on their own (Catalino, 2015). Levinson (2014) looked at hospital emergency response during Hurricane Sandy. Phillips (2018) discussed the EP managers stress, and burnout during disaster deployment. Phillips (2018) used a secondary data set in her quantitative correlation study, with n = 4776. Main questions related to physiological demands on the job, stress on the job, and peer support in the form of offering psychological first aid (Phillips, 2018). Linear regression was used as a statistical analysis (Phillips, 2018). Results included a significant relationship between burning out, job demands, and perceived stress during disaster deployment (Phillips, 2018). Results for peer support and burnout did not find a significant correlation which contradicts prior research (Phillips, 2018).
Melnikov, Itzhaki and Kagan (2014) explored the willingness of Israeli nurses to respond to a disaster. It is an important element in disaster planning to know how many staff will be available to respond and willing to come to work when needed (Melnikov et al., 2014). The authors used a convenience sample of n = 243 nurses who answered surveys. Data analysis included descriptive statistical elements, Pearson correlation coefficients, t-tests and multiple regression analysis (Melnikov et al. 2014). The study found that there is an educational element that need to be added for nurses including self-efficacy. From the nurses who filled out the survey, less than half of them reported to work in prior cases when responding to a disaster (Melnikov et al., 2014). Causes of not reporting included, but not limited to, childcare issues, knowledge, intention to report to work and self-efficacy (Melnikov et al. 2014). Nurses who had higher efficacy on the survey were more likely to respond to disasters (Melnikov et al. 2014). Errett et al. (2013) explored the willingness of Medical Reserve Corps (MRC) volunteers to respond to disasters that are public health related. The MRC has over 200,000 volunteers nationwide with a role of supporting public health workforce and the community during and after a disaster (Errett, et al. 2013). The participants filled out an online survey n = 3181 (Errett et al. 2013). The authors explored four different scenarios including a radiological event, pandemic influenza, weather related event and bioterrorism scenario (Errett et al. 2013). The researchers found that responders with higher self-efficacy were more likely to respond to disasters than those with low self-efficacy (Errett et al. 2013). The study concluded that even volunteers 1 out of 10 who signed up for disaster response might not have the willingness respond to a disaster (Errett et al. 2013). Errett et al. (2013) outlined that the findings of the study were similar to other findings of staff willingness response related to disasters in hospitals, public health sector, and emergency medical technicians.
Rivera-Rodriguez (2017) explored public health nurse's role and preparedness during disasters by using a systematic literature review. The author described difficulties for nurses to respond related to fear, not knowing what to do in a disaster, and worries about their families (Rivera-Rodriguez, 2017). It is important for nurses to understand their role, and what way they need to do to respond during a disaster (Rivera-Rodriguez, 2017). Findings included that there is not enough evidence to define the role of public health nurses, during a disaster and additional research is needed in this area (Rivera- Rodriguez, 2017). This literature raises the question on responsiveness to emergencies and disasters, when there is no clear role definition for nurses in public health. Luscumb (2017) in a literature review about nurses' willingness to respond to earthquakes, found that it is essential for nurses to be available during a disaster response, for the local hospitals to succeed. Nurses willingness to respond dependent upon having children, elderly or disabled family members at home, fear of becoming ill or having a family member who is ill (Luscumb, 2017). Having childcare is another factor when looking at nurses caring for others in a disaster (Luscumb, 2017). Ben Natan, Nigel, Yevdayev, Qadan and Dudkiewicz (2013) explored nurses' willingness to report for work in the event of earthquake in Israel. The researchers found that 57% of respondents were willing to report to work in case of an earthquake (Ben Natan et al. 2013). The researchers used self-administered surveys for n = 400 nurses (Ben Natan et al. 2013). Predictors to report to work included increased self - efficacy, nurses experience, available support including multi-disciplinary collaboration, and level of knowledge (Ben Natan et al. 2013). Based on the finding's hospitals can work on supporting nurses, this action can increase likelihood for nurses willing to report to work during a disaster.
Boyd et al. (2017) looked at the CDC's Emergency Response and Recovery Branch (ERRB) humanitarian emergencies and public health response in the years 2010–2016. Case studies included Haiti earthquake response in 2010, Horn of Africa famine and displacement response 2011–2014 and Syria displacement response from 2012 to present (Boyd et al. 2017). Findings included the need for close relationship and collaboration with other agencies and organizations, and epidemiologic methods that function in an environment where resources are limited (Boyd et al. 2017). Additional findings included the need to be flexible to the population and situation at hand, commitment to support the community long term and the expertise of people who had been in disaster responses before (Boyd et al. 2017).
Communication
Liu et al. (2016) described communication with the public based on four elements: understanding the message, believing of the information presented, personalizing the message and deciding on what actions to take. Paek, Hilyard, Freimuth, Barge and Mindlin (2010) in their article theory-based approaches to understanding public emergency preparedness: implications for effective health and risk communication examined theory-based approaches like the Transtheoretical Model (TTM) in EP to recognize the effectiveness in communication. The study used TTM in two ways including the use of model for the dependent variable by creating a measurement for EP actions (Paek, et al. 2010). The second way was to look at theoretical concepts that are crucial to EP (Paek, et al. 2010). The study method included random digit telephone surveys using multistage sampling method (Paek, et al. 2010). The study found that 24% individuals are in action stage and 30.5% are in maintenance based on the TTM model in their stages of EP (Paek, et al. 2010). The article supports the usefulness of the TTM as a framework in EP analysis for individual responses (Paek, et al. 2010).
Palttala, Boano, Lund, and Vos (2012) looked at crisis communication gaps in disaster management, by using qualitative open-ended questions. The authors established that during crisis, communication must be quick, and effective (Palttala et al. 2012). The online qualitative questions had 40 responses that were analyzed by deep content analysis, seeking emerging themes (Palttala et al. 2012). Communication gaps identified included: coordination and cooperation regarding communication within the disaster response network, with media and with citizens (Palttala et al. 2012). The authors recommended future research as communication patterns and effectiveness varies across countries (Palttala et al. 2012). Liu, Fraustino and Jin. (2016) looked at social media and its role in disaster response and communication. Liu et al. (2016) describes 72% of the population using social media like Facebook or MySpace. Sandborn (2017) in her report on Hurricane Harvey described difficulties in communication, with state and federal officials. Additional difficulties included, providing shelters for all people needed, taking care people with disabilities, and taking care dialysis patients (Sandborn, 2017). Obaid et al. (2017) found that communication that is well planned between multiple agencies during a disaster creates a valuable strength for coordination during a disaster.
Liu et al. (2018) looked at communication during disasters in a hospital setting. The authors used snowball sampling and had interviewed 27 people in crisis management or communications experience in a hospital setting (Liu et al. 2018). The authors stopped interviewing once their data reached saturation of same themes, coming up with no additional emerging themes (Liu et al. 2018). Liu et al. (2018) used a qualitative data program to code their transcripts and looked for emerging themes. Examples of themes: avoid over sharing of information, segment communication, care first, emphasize local ties, face to face communication and nurse empowerment (Liu et al. 2018). Findings included the need to reinforce current best practices, managing up, looking at better communication with media outlets (Liu et al. 2018). Anthony, Sellnow and Millner (2013) described effective crisis communication when people can make the best reasonable choice possible, based on the gathered information. The researchers used 8 focus groups, to determine the use of message convergence framework effectiveness in crisis communication (Anthony et al. 2013). Internal communication issues can cause problems during disasters. Liu et al., (2018) found that delayed internal risk communication can threaten the wellbeing of both staff, and patients. Another problem is miscommunication during a disaster, that can create wrong actions from hospital staff (Liu et al. 2018). Solutions could include correcting the information, there is future research needed in this area what would be the best practice for success (Liu et al. 2018). Receiving the proper information from credible sources during a disaster help people choose proper actions based on the received information (Anthony et al. 2013). Liu et al (2016) conducted an online study with n = 2015 participants via random national sample. The survey included a Linkert scale looking at information sharing behavior and taking protective actions (Liu et al. 2016). The finding included that people predominantly prefer phone conversations, and face to face interactions, e-mailing, and texting instead of social media communication (Liu et al. 2016).
Woods (2016) used a case study approach to look at two hospital's responses after getting Ebola patients. Woods (2016) used thematic textual analysis with inductive category development. Themes found included planning, practice, protocols, collaboration, communication and reassurance (Woods, 2016). Findings of the study included that at one of the hospitals ineffective communication led to misdiagnosis and death (Woods, 2016). Additional problems included, inadequate practice and training on how to use protective equipment for Ebola patients (Woods, 2016). The study outlined the importance of effective communication needs, among hospital staff. In this case proper communication that was timely could have prevented misdiagnosis and death.
Gaps in Literature
Hammad, Arbon, Gebbie and Hutton (2017) used a hermeneutic phenomenological approach in their qualitative inquiry, interviewing 13 nurses from all over the world including the United States. The authors used thematic analysis for their data (Hammad et al. 2017). The research identified five themes including notification, waiting, patient arrival, carrying for patients and reflection (Hammad et al. 2017). Findings included that education for nurses to prepare for disasters and additional research needed for disaster preparedness (Hammad et al. 2017). The article showed the gap in the literature for EP (Hammad et al. 2017). Baack and Alfred (2013) described the need to research nurse's role during a disaster. The authors concur that there is only a small amount of research in this area. The research is highly needed as nurses consist of the largest workforce in the healthcare system (Baack & Alfred, 2013). The authors described nurses as being involved in each part of disaster and preparedness planning (Baack & Alfred, 2013).
Liu et al. (2018) in their qualitative study found that there is a need for research in the literature, related to crisis communication, for nursing staff in hospitals. Liu et al. (2018) suggested that nurses can play a key role in crisis communication, related to the trusted relationship between nurses, and patients, and their families. Additional research needed in face to face communication, and best practices during a disaster (Liu et al. 2018). Liu et al. (2018) found that most communications in hospitals happen face to face, and currently to the authors knowledge there is no research being done in this area. Liu at al. (2016) described a future research need into social media communication, and the reasons why people prefer other means of communications in disaster, like phone calls, and face to face communication instead of using social media. Gossip et al. (2017) in her rapid realist review and Savoia et al. (2017), in their systematic literature review found that there is a gap in the literature regarding information-sharing between organizations including public health departments sharing findings, updating key stakeholders and communication with the public, including creating information for diverse audiences. Gossip et al. (2017) suggest that future studies needed to explore how current technology can help disseminate information learned from previous disasters to improve future responses. Phillips (2018) concluded that there is little research in exploring burnout and stress, in emergency managers deployed during a disaster. Rivera - Rodriguez (2016) described the gap in the literature to define the roles of public health nurse during a disaster.
Alim et al. (2015) found that there is a gap in the literature that requires need for disaster training development for nursing students and post training short- and long-term evaluation of effectiveness of EP training. Pourvakhshoori, Norouzi, Ahmadi, Hosseini, and Khankeh (2017) reviewed literature on disaster nursing. Pourvakhshoori et al. (2017) identified nurses as health care professionals playing a key role in the outcome of disasters. The authors while searching for a model for nurses that can be used in disasters have found that there is no comprehensive model at this time and there is a need for further research to identify or develop a comprehensive model for nurses that can be used during disasters (Pourvakhshoori et al. 2017). Pourvakhshoori et al. (2017) described the necessity to develop a disaster preparedness nursing model to increase better outcomes from preparation to response.
Conclusion
Disasters can happen at any time in any area of the United States. EP is essential to help respond to manmade and natural disasters. Hospitals are essential entities to respond to emergencies during disasters as they are the front line of support in the community (Liu et al. 2018). The complexity of preparing for disasters includes many elements that need to be coordinated. EP managers in hospitals are key personal to support the preparedness and response process to disasters. EP managers are at high risk for burnout, related to physical demands, and stress during deployment (Phillips, 2018). There were gaps found in certain elements of preparedness, based on the above literature review. Coordination and preparation efforts for emergencies, related to disasters, can include but not limited to effective communication strategies, including risk communication, communication is disasters both internally and with outside agencies, appropriate training and practice for staff and community, available equipment, resources, previously developed policies and response protocols (Anthony et al. 2013; Liu et al. 2018; Woods, 2016). Lanard and Sandman (2014) are risk communicators who warn about the need for education of the public and more open communication regarding pandemic diseases. Gossip et al. (2017) described the need for disaster risk reduction related to the cost of disasters with natural disasters costing more than $1.3 trillion in the US, affecting a billion and a half people and causing 700,000 deaths in the last decade. VanVactor (2016) suggested building relationships, braking down silos between organizations, improving effectiveness and efficiency of logistics during disasters related to the cost 60–80% in a disaster is due to getting supplies where and when they are needed. Based on the above findings in the current literature in the past 5–10 years there is a need for future exploration of the experiences of EP managers in rural areas in the Pacific Northwest to fill the current knowledge gap. Chapter 2 included an introduction, literature search strategies, a detailed theoretical framework on complexity theory, a detailed literature review on EP and a conclusion. Chapter 3 provides an introduction, information on the research design, nature of the study with a rationale, participant selection, instrumentation, sources of data, interview questions, research analysis, participant's rights, and a chapter summary.
Doctoral Dissertation Originally published by Walden University 2019 Walden University College of Health Sciences
Review Committee
Dr. Frazier Beatty, Committee Chairperson, Public Health Faculty
Dr. German Gonzalez, Committee Member, Public Health Faculty
Dr. Melissa Green, University Reviewer, Public Health Faculty
Chief Academic Officer
Eric Riedel, Ph.D. Walden University 2019
References
Ablah, E., Konda, K. S., Konda, K., Melbourne, M., Ingoglia, J. N., & Gebbie, K. M. (2010). EP training and response among community health centers and local health departments: results from a multi-state survey. Community Health, 35(3), 285–293. doi: 10.1007/s10900–010–9236–7
Adini, B., Laor, D., & Aharonson-Daniel, L. (2014). Factors affecting preparedness and capacity to manage pandemic influenza: perceptions of healthcare managers. Public Health, 128(8), 703–708. doi: 10.1016/j.puhe.2014.06.002
Alim, S., Kawabata, M., & Nakazawa, M. (2015). Evaluation of disaster preparedness training and disaster drill for nursing students. Nurse Education Today, 35(1), 25–31. doi: 10.1016/j.nedt.2014.04.016
Alzahrani, F., & Kyratsis, Y. (2017). Emergency nurse disaster preparedness during mass gatherings: a cross-sectional survey of emergency nurses' perceptions in hospitals in Mecca, Saudi Arabia. BMJ Open, 7(4), e013563. doi:10.1136/bmjopen-2016–013563
Anthony, K. E., Sellnow, T. L., & Millner, A. G. (2013). Message convergence as a message-centered approach to analyzing and improving risk communication. Applied Communication Research, 41(4), 346–364. http://dx.doi.org/10.1080/00909882.2013.844346
Baack, S., & Alfred, D. (2013). Nurses' preparedness and perceived competence in managing disasters. Nursing Scholarship: An Official Publication of Sigma Theta Tau International Honor Society of Nursing, 45(3), 281–287. http://dx.doi.
org/10.1111/jnu.12029. doi: 10.1111/jnu.12029
Baker, S. E., Edwards, R., & Doidge, M. (2012). How many qualitative interviews is enough? Expert voices and early career reflections on sampling and cases in qualitative research. Retrieved from National Centre for Research Methods: http://eprints.ncrm.ac.uk/2273/4/how_many_interviews.pdf
Bennett, D. Phillips, B.D. & Davis, E. (2017, March). The future of accessibility in disaster conditions: How wireless technologies will transform the life cycle of emergency management, Futures, 87, 122–132, https://doi.org/10.1016/j.futures.2016.05.004
Ben Natan, M., Nigel, S., Yevdayev, I., Qadan, M., & Dudkiewicz, M. (2013). Nurses' willingness to report for work in the event of earthquake in Israel. Journal of Nursing Management. doi:10.1111/jonm.12058
Bin Shalhoub, A. A., Khan, A. A., & Alaska, Y. A. (2017). Evaluation of disaster preparedness for mass casualty incidents in private hospitals in Central Saudi Arabia. Saudi Medical, 38(3), 302–306. doi:10.15537/smj.2017.3.17483
Bornmann, L. (2013). What is social impact of research and how can it be assessed? A literature survey. American Society for Information Science and Technology, 64. 10.1002/asi.22803.
Boyd, A. T., Cookson, S. T., Anderson, M., Bilukha, O. O., Brennan, M., Handzel, T….Gerber, M. (2017). Centers for Disease Control and Prevention public health response to humanitarian emergencies, 2007–2016. Emerging Infectious Diseases, 23(13). https://dx.doi.org/10.3201/eid2313.170473
Brand, S. L., Fleming, L. E., & Wyatt, K. M. (2015). Tailoring healthy workplace interventions to local healthcare settings: A Complexity Theory-Informed workplace of well-being framework. The Scientific World, 340820. doi:10.1155/2015/340820
Browne, N.M. & Keeley, S.M. (2007). Asking the Right Questions. A guide to critical thinking. Upper Saddle River, NJ: Pearson Education.
Byng, R., & Jones, R. (2004). Mental health link: the development and formative evaluation of a complex intervention to improve shared care for patients with long-term mental illness. Journal of Evaluation in Clinical Practice, 10(1), 27–36.
Cagliuso, N. V. (2014). Stakeholders' experiences with US hospital emergency preparedness: Part 1. Business Continuity & Emergency Planning, 8(2), 156–168.
Cagliuso, N. S. (2014a). Stakeholders' experiences with US hospital emergency preparedness - Part 2. Business Continuity & Emergency Planning, 8(3), 263–279.
Cagliuso, N. V. (2012). Stakeholders' experiences with U.S. hospital EP (Order №3519439). Available from Dissertations & Theses @ Walden University.
Catalino, J., Jr. (2015). The impact of federal emergency management legislation on at-risk and vulnerable populations for disaster preparedness and response (Order №3702737). Available from Dissertations & Theses @ Walden University. (1686122879).
Charney, R., Rebmann, T., & Flood, R. B. (2014). Working after a tornado: a survey of hospital personnel in Joplin, Missouri. Biosecurity and Bioterrorism: Biodefense Strategy, Practice and Science, 12(4), 190–200. http://dx.doi.org/10.1089/bsp.2014.0010
Christian, M. D., Kollek, D., & Schwartz, B. (2005). Emergency preparedness: What every health care worker needs to know. CJEM: Canadian Association of Emergency Physicians, 7(5), 330–7.
Cirkovic, M., Sandberg, A., & Bostrom, N. (2010). Anthropic shadow: observation selection effects and human extinction risks. Risk Analysis: International, 30(10), 1495–1506. doi: 10.1111/j.1539–6924.2010. 01460.x
Comfort, L. (1995). Self-organization in disaster response and recovery. The Maharashta, India, earthquake of September 30, 1993. Natural Hazards Research and Applications Information Center, Quick Response Reports №74. University of Colorado, Boulder, Colorado. Retrieved from https://scholarcommons.usf.edu/cgi/viewcontent.cgi?referer=https://www.google.com/&httpsredir=1&article=1041&context=fmhi_pub
Creswell, J. W. (2014). Qualitative, quantitive, and mixed methods approaches. Thousand Oaks, CA: Sage Publications.
de Cassia Nunes Nascimento, L., Vignuda de Souza, T., Oliveira, I. S., de Montenegro Medeiros de Moraes, J. R., Cordeiro Burla de Aguiar, R., & Faria da Silva, L. (2018). Theoretical saturation in qualitative research: an experience report in interview with schoolchildren. Revista Brasileira De Enfermagem, 71(1), 228–233. doi:10.1590/0034–7167–2016–0616
Egli. D. S. (2013). Beyond the storms: strengthening preparedness, response, & resilience in the 21st century. Strategic Security, 6 (2),32–45 (2013), doi: 10.5038/1944–0472.6.2.3
Egli, D. S. (2014). Beyond the storms: strengthening homeland security & disaster management to achieve resilience. Homeland Security Review, (1), 101.
Elko, J. (2017). CMS EP rule: required processes to have in place: make sure your organization has processes in place as soon as possible. Health Care Compliance, 19(6), 25–58.
Encyclopedia Britannica. (2019). Pacific Coast, region, North America. Retrieved from https://www.britannica.com/place/Pacific-Coast
Errett, N. A., Barnett, D. J., & Thompson, C. B., et al. (2013). Assessment of medical reserve corps volunteers' emergency response willingness using a threat- and efficacy-based model. Biosecurity Bioterror,11(1):29–40. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3612278/
Fagbuyi, D. B., Schonfeld, D. J., Krug, S. E., Chung, S., Fisher, M. C., Needle, S. M., & Disaster Preparedness Advisory. (2016). Medical countermeasures for children in public health emergencies, disasters, or terrorism. Pediatrics, 137(2). doi: 10.1542/peds.2015–4273
Goss, T. (2017). Emergency managers' perceptions of all-hazards pandemic planning effectiveness in north Texas (Order №10641382). Available from Dissertations & Theses @ Walden University. (1970753944).
Gossip, K., Gouda, H., Yong Yi Lee, Firth, S., Bermejo III, R., Zeck, W., … Jimenez Soto, E. (2017). Monitoring and evaluation of disaster response efforts undertaken by local health departments: a rapid realist review. BMC Health Services Research, 17, 1–11. https://doi-org.ezp.waldenulibrary.org/10.1186/s12913-017-2396-8
Guest, G., Bunce, A., & Johnson, L. (2006). How many interviews are enough? An experiment with data saturation and variability. Field Methods, 18(1), 59–82. doi:10.1177/1525822X05279903
Halcomb, E. J., & Davidson, P. M. (2006). Is verbatim transcription of interview data always necessary? Applied Nursing Research, 19(1), 38–42. doi: 10.1016/j.apnr.2005.06.001
Hammad, K. S., Arbon, P., Gebbie, K., & Hutton, A. (2017). Moments of disaster response in the emergency department (ED). Australasian Emergency Nursing, 20(4), 181–185. doi: 10.1016/j.aenj.2017.10.002
Hilhorst, D. (2003). Responding to disasters. Diversity of bureaucrats, technocrats and local people. International Mass Emergencies and Disasters, 21(1), 37–56.
Hodge, A. J., Miller, E. L., & Dilts Skaggs, M. K. (2017). Nursing self-perceptions of EP at a rural hospital. JEN: Emergency Nursing, 43(1), 10–14. doi: 10.1016/j.jen.2015.07.012
Hodge, J., G, Jr, & Gostin, L., O. (2017). Revamping the us federal common rule: Modernizing human participant research regulations. JAMA, 317(15), 1521–1522. Retrieved from http://dx.doi.org/10.1001/jama.2017.1633
IFRC (n.d.). Types of disasters: Definition of hazards. Retrieved from https://www.ifrc.org/en/what-we-do/disaster-management/about-disasters/definition-of-hazard/
Jacob, S. A., & Furgerson, S. P. (2012). Writing interview protocols and conducting interviews: tips for students new to the field of qualitative research. The Qualitative Report,17(42), 1–10. Retrieved from http://nsuworks.nova.edu/tqr/vol17/iss42/3
Jovchelovitch, S., Bauer, M. W., (2000) Narrative interviewing. In M. W. Bauer, and G. Gaskell,., (Eds.). Qualitative researching with text, IMAge and Sound: a practical handbook (pp. 57–74). London, UK: SAGE.
Kaji, A. H., Koenig, K. L., & Lewis, R. J. (2007). Current hospital disaster preparedness. Journal of the American medical association, 298(18), 2188–2190.
Kezar, A. k. (2014). Higher education change and social networks: A review of research. Higher Education, 85(1), 91–125.
Laureate Education (Producer). (2015). Social impact of a dissertation [Video file]. Baltimore, MD: Author.
Laureate Education (Producer). (2016, a). First cycle coding: Structural coding [Video file]. Baltimore, MD: Author.
Laureate Education (Producer). (2017). Voices from the field [Interactive media]. Baltimore, MD: Author.
Lanard, J., & Sandman, P. M. (2014). Ebola: Failures of imagination. Retrieved from http://psandman.com/col/Ebola-3.htm.
Landman, A., Teich, J. M., Pruitt, P., Moore, S. E., Theriault, J., Dorisca, E., et al. (2015). The Boston marathon bombings mass casualty incident: one emergency
department's information systems challenges and opportunities. Annals of Emergency Medicine, 66(1), 51–59. http://dx.doi.org/10.1016/j.ann emergmed.2014.06.009
Leider, J. P., DeBruin, D., Reynolds, N., Koch, A., & Seaberg, J. (2017). Ethical guidance for disaster response, specifically around crisis standards of care: A systematic review. American Public Health, 107(9), e1–e9. https://doi-org.ezp.waldenulibrary.org/10.2105/AJPH.2017.303882
Levinson, D. L. (2014). Hospital EP and response during superstorm Sandy. U. S. Department of Health and Human Services, Washington, DC. Retrieved from: http://oig.hhs.
gov/oei/reports/oei-06–13–00260.pdf
Liu, B. F. Fowler, B. M., Roberts, H. A., & Herovic, E. (2018). Keeping hospitals operating during disasters through crisis communication preparedness. Public Relations Review, 44(4), 585–597. doi: 10.1016/j.pubrev.2018.06.002
Liu, B. F., Fraustino, J. D., & Jin, Y. (2016). Social media use during disasters: How information form and source influence intended behavioral responses. Communication Research, 43(5), 626–646. http://dx.doi.org/10.1177/0093650214565917
Long, K. M., McDermott, F., & Meadows, G. N. (2018). Being pragmatic about healthcare complexity: our experiences applying complexity theory and pragmatism to health services research. BMC Medicine, 16(1), 94. https://doi-org.ezp.waldenulibrary.org/10.1186/s12916-018-1087-6
Luscumb, J. M. (2017). Willingness of nurses to respond after Alaskan earthquake: Systematic literature review (Order №10257330). Available from Dissertations & Theses @ Walden University. (1896557477).
Lucchini, R. G., Hashim, D., Acquilla, S., Basanets, A., Bertazzi, P. A., Bushmanov, A., & … Todd, A. C. (2017). A comparative assessment of major international disasters: the need for exposure assessment, systematic emergency preparedness, and lifetime health care. BMC Public Health, 17(1), 46. doi:10.1186/s12889–016–3939–3
Markiewicz, M., Bevc, C. A., Hegle, J., Horney, J. A., Davies, M., & MacDonald, P. M. (2012). Linking public health agencies and hospitals for improved emergency preparedness: North Carolina's public health epidemiologist program. BMC Public Health, 12,141. doi:10.1186/1471–2458–12–141
Martin, E., Nolte, I., & Vitolo, E. (2016). The four Cs of disaster partnering: Communication, cooperation, coordination and collaboration. Disasters, 40(4), 621–643. http://dx.doi.org/10.1111/disa.12173
Mason, M. (2010). Sample size and saturation in PhD studies using qualitative interviews. Forum Qualitative Sozialforschung/Forum: Qualitative Social Research, 11(3), article 8. Retrieved from http://www.qualitative-research.net/index.php/fqs
Math, S. B., Nirmala, M. C., Moirangthem, S., & Kumar, N. C. (2015). Disaster management: mental health perspective. Indian Psychological Medicine, 37(3), 261–271.
McDermott, S., Martin, K., & Gardner, J. D. (2016). Disaster response for people with disability. Disability and Health, 9(2), 183–185. https://doi-
Melnikov, S., Itzhaki, M., & Kagan, I., (2014). Israeli nurses' intention to report for work in an emergency or disaster. Nursing Scholarship, 46(2), 134–42. doi: 10.1111/jnu.12056
Mellow, M. A., Bloch, D., & Grimes, J. (2018). The CMS final rule for EP implementation deadline is here: Is your facility prepared? Defense Counsel, 85(1), 1–5.
Murthy, B. P., M. Molinari, N., LeBlanc, T. T., Vagi, S. J., & Avchen, R. N. (2017). Progress in public health emergency preparedness - United States, 2001–2016. American Public Health, 107S180-S185. doi:10.2105/AJPH.2017.304038
Myers, D. M., & Neuman, M. (2007). The qualitative interview in IS research: Examining the craft. Information and Organization, 17(1), 2–26.
Nelson, C., Lurie, N., Wasserman, J., & Zakowski, S. (2007). Conceptualizing and defining public health emergency preparedness. American journal of public health, 97 Suppl 1(Suppl 1), S9–11.
North, C.S. & Pfefferbaum, B. (2013). Mental Health Response to Community Disasters A Systematic Review. Journal of American Medical Association. 2013;310(5):507–518. doi:10.1001/jama.2013.107799
NVivo (2019). Organize material into themes with coding in NVivo 9. NVivo Tutorial Video. Retrieved from https://www.youtube.com/watch?v=O9eTvP3E5TE
NVivo (2019, a). Find themes and analyze text in NVivo 9. NVivo Tutorial Video. Retrieved from https://www.youtube.com/watch?v=ypo6lrpwDZ8
Obaid, J. M., Bailey, G., Wheeler, H., Meyers, L., Medcalf, S. J., Hansen, K. F., . . . Lowe, J. J. (2017). Utilization of functional exercises to build regional EP among rural health organizations in the US. Prehospital and Disaster Medicine, 32(2), 224–230. doi: http://dx.doi.org.ezp.waldenulibrary.org/10.1017/S1049023X16001527
Federal Register US (2016). Medicare and Medicaid programs; EP requirements for Medicare and Medicaid participating providers and suppliers. Retrieved from https://www.federalregister.gov/documents/2016/09/16/2016-21404/medicare-and-medicaid-programs-emergency-preparedness-requirements-for-medicare-and-medicaid
OHSU Oregon Office of Rural Health (2019). Rural and frontier hospitals. Retrieved from https://www.ohsu.edu/xd/outreach/oregon-rural-health/rural-frontier-facilities/hospitals/index.cfm
OHSU Oregon Office of Rural Health (2019, a). Directory of Rural and frontier hospitals. Retrieved from https://www.ohsu.edu/xd/outreach/oregon-rural-health/rural-frontier-facilities/hospitals/hospital-directory.cfm
Oregon Demographics (2019). Oregon counties by population. Retrieved from https://www.oregon-demographics.com/counties_by_population
Oregon Health Authority (n.d.). Current hazards. Health security, preparedness, and response. Retrieved from http://www.oregon.gov/oha/PH/PREPAREDNESS/CURRENTHAZARDS/Pages/index.aspx
Oregon Health Authority (n.d., a). Providers/suppliers facilities impacted by the EP rule. Retrieved from https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertEmergPrep/Downloads/17-Facility-Provider-Supplier-Types-Impacted.pdf
Paganini, M., Borrelli, F., Cattani, J., Ragazzoni, L., Djalali, A., Carenzo, L., & … Ingrassia, P. L. (2016). Assessment of disaster preparedness among emergency departments in Italian hospitals: a cautious warning for disaster risk reduction and management capacity. Scandinavian Trauma, Resuscitation and Emergency Medicine, 24(1), 101. doi:10.1186/s13049–016–0292–6
Patton, M. Q. (2015). Qualitative research & evaluation methods: Integrating theory and practice (4th ed.). Thousand Oaks, CA: SAGE.
Paek, H., Hilyard, K., Freimuth, V., Barge, J., & Mindlin, M. (2010). Theory-based approaches to understanding public emergency preparedness: implications for effective health and risk communication. Health Communication, 15(4), 428–444. doi:10.1080/10810731003753083
Paganini, M., Borrelli, F., Cattani, J., Ragazzoni, L., Djalali, A., Carenzo, L., & … Ingrassia, P. L. (2016). Assessment of disaster preparedness among emergency departments in Italian hospitals: a cautious warning for disaster risk reduction and management capacity. Scandinavian Trauma, Resuscitation and Emergency Medicine, 24(1), 101. doi:10.1186/s13049–016–0292–6
Paley, J., & Eva, G. (2011). Complexity theory as an approach to explanation in healthcare: a critical discussion. International Nursing Studies, 48(2), 269–279. doi: 10.1016/j.ijnurstu.2010.09.012
Palttala, P., Boano, C., Lund, R., & Vos, M. (2012). Communication gaps in disaster management: perceptions by experts from governmental and non-governmental organizations. Contingencies & Crisis Management, 20(1), 2–12. https://doi-org.ezp.waldenulibrary.org/10.1111/j.1468-5973.2011.00656.x
Phillips, A. H. (2018). Exploring burnout and perceived stress in emergency managers during deployments (Order №10748976). Available from Dissertations & Theses @ Walden University. (2027325598).
Plsek, P. E., & Greenhalgh, T. (2001). Complexity science: The challenge of complexity in health care. BMJ (Clinical Research Ed.), 323(7313), 625–628.
Pourvakhshoori, N., Norouzi, K., Ahmadi, F., Hosseini, M., & Khankeh, H. (2017). Nursing in disasters: A review of existing models. International Emergency Nursing, 31, 58–63. doi: 10.1016/j.ienj.2016.06.004
Rahm, D., & Reddick, C. G. (2011). US city managers' perceptions of disaster risks: consequences for urban emergency management. Contingencies & Crisis Management, 19(3), 136–146. doi: 10.1111/j.1468–5973.2011.00647.x
Ramsey Hamilton, C., & Miller, D. (2017). The new CMS EP final rule and its impact on healthcare in 2017. Healthcare Protection Management, 33(1), 77–81.
Ravitch, S. M., & Carl, N. M. (2016). Qualitative research: Bridging the conceptual, theoretical, and methodological. Thousand Oaks, CA: Sage Publications.
Reed, J. E., Howe, C., Doyle, C., & Bell, D. (2018). Simple rules for evidence translation in complex systems: A qualitative study. BMC Medicine, 16(1), 92. https://doi.org/10.1186/s12916-018-1076-9
Ripoll Gallardo, A., Djalali, A., Foletti, M., Ragazzoni, L., Della Corte, F., Lupescu, O., . . . Ingrassia, P. (2015). Core competencies in disaster management and humanitarian assistance: A systematic review. Disaster Medicine and Public Health Preparedness, 9(4), 430–439. doi:10.1017/dmp.2015.24
Rivera-Rodriguez, E. (2017). Role of the nurse during disaster preparedness: A systematic literature review and application to public health nurses (Order №10636520). Available from Dissertations & Theses @ Walden University. (1964397933).
Roets, L. (2017). Protection of the human research participant: A structured review. South African Medical, 107(10), 847–853. doi:10.7196/SAMJ. 2017.v107i10.12533
Rowlands, T., Waddell, N., & Mckenna, B. (2015). Are we there yet? A technique to determine theoretical saturation. Computer Information Systems, 56(1), 40–47.
Rubin, H. J., & Rubin, I. S. (2012). Qualitative interviewing: The art of hearing data (3rd ed.). Thousand Oaks, CA: SAGE.
Rudestam, K. E., & Newton, R. R. (2015). Surviving your dissertation: A comprehensive guide to content and process (4th ed.). Thousand Oaks, CA: Sage.
Sandborn, B. (2017). Hurricane Harvey lessons are a roadmap for hospital disaster response. Healthcare Finance. Retrieved from http://www.
healthcarefinancenews.com/news/hurricane-harvey-lessons-are-roadmap-hospital-disaster-response.
Sargeant, J. (2012). Qualitative research part II: Participants, analysis, and quality assurance. Journal of Graduate Medical Education, 4(1), 1. doi:10.4300/JGME-D-11–00307.1
Savoia, E., Lin, L., Bernard, D., Klein, N., James, L. P., & Guicciardi, S. (2017). Public health system research in public health EP in the United States (2009–2015): Actionable knowledge base. American Public Health, 107e1-e6. doi:10.2105/ AJPH.2017.304051
Seale, G. S. (2010). EP as a continuous improvement cycle: perspectives from a postacute rehabilitation facility. Rehabilitation Psychology, 55(3), 247–254. doi:10.1037/a0020599
Seidman, I. (2012). Interviewing as qualitative research: A guide for researchers in education and the social sciences (3rd ed.). New York, NY: Teachers College.
Shah, G. H., Newell, B., & Whitworth, R. E. (2016). Health departments' engagement in EP activities: The influence of health informatics capacity. International Health Policy & Management, 5(10), 575–582. doi: 10.15171/ijhpm.2016.48
Shento, A. K. (2004). Strategies for ensuring trustworthiness in qualitative research projects. Education for Information, 22(2), 63–75. Retrieved from https://pdfs.semanticscholar.org/452e/3393e3ecc34f913e8c49d8faf19b9f89b75d.pdf
Shipman, S. J., Stanton, M. P., Tomlinson, S., Olivet, L., Graves, A., McKnight, D., & Speck, P. M. (2016). Qualitative analysis of the lived experience of first-time nurse responders in disaster. Continuing Education in Nursing, 47(2), 61–71
Smith, J., & Firth, J. (2011). Qualitative data analysis: the framework approach. Nurse Researcher, 18(2), 52–62.
Sobelson, R. K., Wigington, C. J., Harp, V., & Bronson, B. B. (2015). A whole community approach to emergency management: Strategies and best practices of seven community programs. Emergency Management (Weston, Mass.), 13(4), 349–357. doi:10.5055/jem.2015.0247
Statistics Solutions (2017). What is credibility in qualitative research and how do we establish it? Retrieved from http://www.statisticssolutions.com/what-is-credibility-in-qualitative-research-and-how-do-we-establish-it/
Sutton, J., & Austin, Z. (2015). Qualitative research: Data collection, analysis, and management. The Canadian Hospital Pharmacy, 68(3), 226–231. doi:10.4212/cjhp. v68i3.1456
Taschner, M. A., Nannini, A., Laccetti, M., & Greene, M. (2017). EP policy and practice in Massachusetts hospitals. Workplace Health & Safety, 65(3), 129–136. doi:10.1177/2165079916659505
Thompson, D. S., Fazio, X., Kustra, E., Patrick, L., & Stanley, D. (2016). Scoping review of complexity theory in health services research. BMC health services research, 16, 87. doi:10.1186/s12913–016–1343–4
Thrift, N. (1999). The place of complexity. Theory, Culture & Society, (3), 31.
Turner, D. W. (2010). Qualitative interview design: A practical guide for novice investigators. The Qualitative Report, 15(3), 754–760. Retrieved from http://nsuworks.nova.edu/tqr/
Valesky, W., Roblin, P., Patel, B., Adelaine, J., Zehtabchi, S., & Arquilla, B. (2013). Assessing hospital preparedness: comparison of an on-site survey with a self-reported, internet-based, long-distance tabletop drill. Prehospital and Disaster Medicine, 28(5), 441–444. doi:10.1017/S1049023X13003580
VanVactor, J. D. (2016). Healthcare logistics in disaster planning and emergency management: A perspective. Business Continuity & Emergency Planning, 10(2), 157–176.
Veenema, T. G., Griffin, A., Gable, A. R., MacIntyre, L., Simons, R. N., Couig, M. P., … Larson, E. (2016). Nurses as leaders in disaster preparedness and response - a call to action. Nursing Scholarship: An Official Publication of Sigma Theta Tau International Honor Society of Nursing, 48(2), 187–200. doi: 10.1111/jnu.12198
Walden University (n.d.). Email - format Consent Form for Practice Interview.
Walden University (n.d., a). Office of research and compliance: IRB requirements for selecting participants.
Wallace, J. R. (2016). Field test of a peer support pilot project serving federal employees deployed to a major disaster. Social Work & Christianity, 43(1), 128–141.
Washington State Department of Health (n.d.) Rural Health. Designated critical access hospitals. Retrieved from https://www.doh.wa.gov/ForPublicHealthandHealthcareProviders/RuralHealth/RuralHealthSystems/CriticalAccessHospitals/DesignatedCriticalAccessHospitals
Washington State Department of Health (n.d., a) Rural Health. Critical access hospitals. https://www.doh.wa.gov/ForPublicHealthandHealthcareProviders/RuralHealth/RuralHealthSystems/CriticalAccessHospitals
Woods, C. L. (2016). When more than reputation is at risk: How two hospitals responded to Ebola. Public Relations Review, 42(5), 893–902. http://dx.doi.org/10.1016/j. pubrev.2016.10.002.
Wood, N. J., Jones, J., Spielman, S., & Schmidtlein, M. C. (2015). Community clusters of tsunami vulnerability in the US Pacific Northwest. Proceedings of the National Academy of Sciences of the United States of America, 112(17), 5354.
World Population Review (2019). Population of cities in Oregon 2019. Retrieved from http://worldpopulationreview.com/states/oregon-population/cities/
Zusman, E. E., & Marghella, P. D. (2013). Disaster management in the era of lean healthcare. Neurosurgery, 72(2), N11-N14. doi: 10.1227/01.neu.0000426210. 89959.f5. Retrieved from https://academic.oup.com/neurosurgery/article/72/2/N11/2417826
About the Creator
Gabriella Korosi
I am a writer, public health professional, a nurse. Creator of connections, spreading positivity. Interests: health/spirituality/positivity/joy/caring/public health/nursing. My goal is to create positive change.https://gabriellakorosi.org




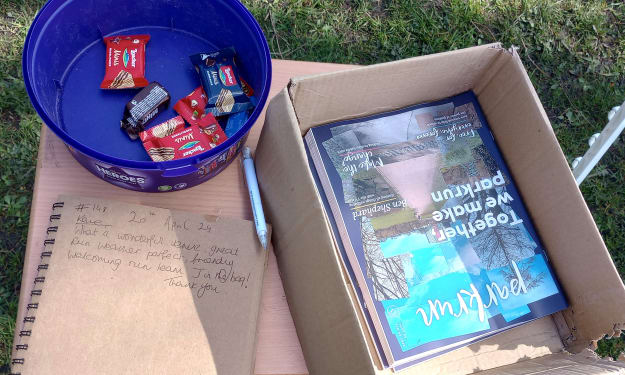


Comments
There are no comments for this story
Be the first to respond and start the conversation.