
STDs can catch anyone who has a love life. Our experts explain how to protect yourself from sexually transmitted diseases and how you can detect and treat a possible infection early.
What are STIs?
STIs are more precisely referred to as "sexually transmitted infections" (STI). The umbrella term stands for infections that you can catch during sex. Because the symptoms of the infections are often difficult to recognize, they are often passed on unknowingly. But don't worry: most STIs are treatable with medication and don't leave permanent damage, as long as they're caught in time. Unfortunately, STIs are still a taboo subject. No one likes to talk about itching or rashes in the crotch, which is why treatment is often started too late and consequential damage is threatened.
How can you get an STD?
Sexually transmitted diseases exist all over the world, some are more common in certain regions than in others. They are caused by bacteria, viruses or fungi. People who have changing sex partners run a higher risk of getting a sexually transmitted infection than people with a steady sex partner. Unprotected sex always carries a risk. The World Health Organization (WHO) has calculated that 1 million people are newly infected every day. Genital herpes alone infects 500 million people worldwide. How exactly an infection is transmitted during sex depends on the type of disease. Possible routes of infection are:
Kissing
Oral sex
Vaginal sex
Anal sex
Petting

How do pathogens of STIs enter the body?
The pathogens enter the body either through body fluids or through pathological skin changes via the warm, moist mucous membranes. These are in fact an ideal breeding ground for the pathogens. They are located at: Mouth, eye, glans, anus, urethra, labia. By the way: Infected sex toys can also be carriers. That's why you should always pay attention to hygiene.
How dangerous are STIs?
Quite apart from the fact that an STI endangers those around you, a disease that is not detected or detected too late can also be life-threatening for you. Infertility, cancer and chronic diseases can be the result. Since an existing infection also damages the mucous membranes, infected persons carry a higher risk of contracting an additional disease.
What diseases are there and how can I recognize them?
An interview with Prof. Dr. Hartmut Porst, a specialist in urology in Hamburg, provides some information:
The condom let you down when you needed it most? And now you're afraid you've contracted an STD? Tip for immediate help: "It can help to urinate, so pathogens are flushed out of the urethra," says Prof. Dr. Porst. Rinse your penis, but don't rub it. Otherwise, you'll drive potential pathogens into small sores.
Symptoms: If bacteria or viruses do manage to infect you with a sexually transmitted disease, the good news is that you'll most likely recognize the infection. Except for HPV and HIV, most STDs are noticeable by burning in the urethra and discharge, and herpes by blisters and ulcers. "Then you should go to the urologist immediately and get tested," Porst says.
Unfortunately, if the symptoms go away, that's not a sign of healing. "The infection can continue, and if you carry it over, there can be secondary damage," says the urologist. And you'd rather not experience those: "Inflammation of the urethra can cause it to narrow and you can have problems urinating," says Porst. It then has to be widened again with a complex operation. In addition, epididymitis can occur, which in the worst case can even lead to infertility. In addition, the pathogens can pass into the blood and cause joint diseases. Therefore: Be sure to have yourself examined if you have symptoms.

Examination: "The urologist takes a urethral swab or tests the ejaculate," says Porst. In a urethral swab, a type of cotton swab is pushed into the urethra and examined in the laboratory. Mixed infections often occur. This means that if you have caught one, the next one is not far away. "The mucous membranes are then more vulnerable and therefore more susceptible to infection," explains the urologist. That's why he advises, "Man should definitely also test for HIV and hepatitis after 3 months." Only after this time can a disease be detected.
And what does such a test cost? The costs are covered by health insurance if symptoms are present. You pay for the HIV test yourself. It costs $10 to $25.
Treatment: "Most STIs are treatable and curable with antibiotics, with the exception of virus-transmitted diseases such as HPV, herpes and HIV/AIDS," says Porst. If the doctor contacted promptly believes that HIV infection is possible, PEP (post-exposure prophylaxis) is offered free of charge to all those with statutory health insurance. The insured person is not reimbursed for the costs. PEP can therefore be a very sensible treatment method, about which every patient should seek advice. HIV is not curable, but, "HIV patients today have an almost normal life expectancy." Treatment for the other STDs takes an average of 7 to 10 days. "The most common STDs include mycoplasma, ureaplasma, chlamydia, HPV and herpes," Porst says.
Think once and never again? Unfortunately, no. "You don't develop immunity to STDs," the urologist explains. And there's more bad news: "During treatment, you shouldn't have sex and you should definitely inform your partner about the infection." Worried about causing a relationship crisis? The urologist knows how you can calm them down: "Chlamydia and mycoplasma, for example, can also be caught in the hot tub," says the expert. Unhygienic public toilets can also be a transmission site. And so that your partner doesn't infect you again next, she should also be treated.
Precaution: "The probability of being infected during sex with commercial ladies is much higher than during a one-night stand." Therefore, especially in the red light milieu: use a condom. To be safe from infections, you should also use contraception during oral sex. You can protect yourself with a latex lick cloth or a condom cut open on the vagina.
These are the most common STDs
According to the World Health Organization, there are about 30 different bacteria, viruses and parasites that can cause infections. The following list includes the most common STDs found in Europe.
Common STD #1: Fungi (mycoses).
Although women are much more often affected by fungal diseases, 10 to 20% of all men also suffer from a fungal infection on the penis.
Symptoms: Itching, dry, red rash in the warm moist fold between the scrotum and thigh. Later, also open, sore skin areas from which fluid oozes; crust formation.
Infection: The villain is the yeast Candida albicans, which is transmitted during unprotected sexual intercourse.
Treatment: "Careful washing and thorough drying as well as powder and fungal ointments, in stubborn cases tablets, are the appropriate treatment," recommends Dr. Haydar Karatepe of the Sexual Medicine Center in Frankfurt am Main.
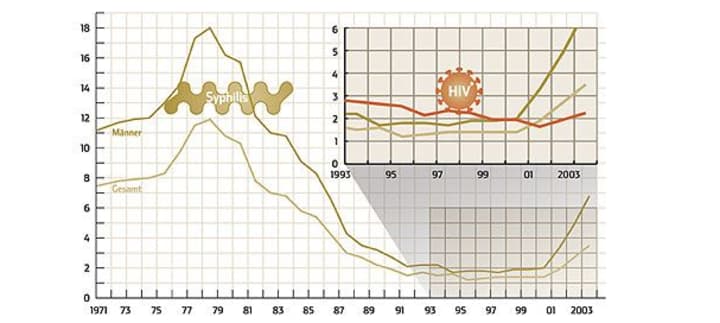
Common STD #2: Syphilis (also: lues, hard chancre).
It used to be called the French disease. Most commonly affects men between the ages of 30 and 40, often through same-sex sex.
Symptoms: The bacterium invades primarily through mucous membranes, i.e., the genitals, anus, and mouth. A hardened ulcer develops there about 3 weeks after infection and the adjacent lymph node swells. Pain usually does not occur in stage I. If left untreated, the disease spreads to the entire body within several weeks to months (stage II). There may be aching limbs, malaise like the flu and rashes that are often misinterpreted as allergies. "However, the symptoms do not have to occur," says Dr. Eva Thoma-Greber, a specialist in sexually transmitted diseases at the Ludwig Maximilian University Dermatology Clinic in Munich. In stage III, the pathogens attack the nervous system, which can lead to neurological symptoms such as headaches and paralysis, and even personality changes.
Infection: Through skin contact with the ulcers, which may also be located within the vagina or rectum, and especially in stage II via semen, vaginal fluid and saliva. Condoms protect to a large extent. Infection via routes other than physical contact (such as a shared towel) is extremely unlikely.
Treatment: the family doctor can determine whether an infection is present with a blood test. "Syphilis responds well to penicillin," Thoma-Greber says. Treatment lasts 2 to 3 weeks. The antibiotic is usually injected, sometimes daily.
Anything else? You can't have sex until the treatment is finished. The doctor must report the disease to the health department (anonymously). Warn your sexual partners. Pregnant women must start therapy early to save their child. Thoma-Greber: "There can be a stillbirth in the worst case."
Common venereal disease #3: Trichomonads.
Trichomonad infection is one of the most common STDs. According to WHO estimates, around 170 million people worldwide become infected with trichomonads every year. Men are much less likely to be affected than women.
Symptoms: Cause milky discharge from the urethra, pulling and itching of the penis, oozing, burning, inflammation of the glans and prostate. Hygiene reduces the risk of infection. If the symptoms are already present, a fairly unproblematic treatment with medication helps.
Infection: Trichomonas infection is caused by the parasite Trichomonas vaginalis. This parasite likes to settle in the warm, moist climate of the vagina and is transmitted to the partner during unprotected sex.
Treatment: The infection is usually cured with 1 week of antibiotic treatment. To protect against re-infection of each other, the partner should also undergo the tablet treatment.
Common STD #4: Chlamydia and Mycoplasma.
Chlamydia infection is one of the most common sexually transmitted diseases. Due to their anatomy, young women are particularly at risk of infection with chlamydia, as their cervix can become infected more easily.

Symptoms: Large urge to urinate and painful urination, mucous-yellowish discharge and stuck urethral outlet in the morning. The infection disappears on its own in about 50% of cases. If it does not, painful abdominal inflammation and infertility due to injury to the vas deferens occur.
Infection: Infection occurs through genital secretions. The spread of chlamydia is increasing. In a study of more than 5000 patients, about 4% were infected, and as high as 9% in women who had contact with 3 to 5 partners in the last 5 years. An infected pregnant woman can also transmit the chlamydia to the newborn during birth.
Treatment: The infection is treated with antibiotics. Depending on the preparation, this is done once or for up to 2 weeks.
What else? Because it is estimated that about 300,000 women become infected with chlamydia in Germany each year and about one-third of them become infertile due to a chlamydia infection, it is recommended for women to have a chlamydia test performed once a year by a gynecologist.
Common venereal disease #5: Genital warts
Along with genital herpes and chlamydia, genital warts, known as condylomas in technical jargon, are among the most common sexually transmitted infections. Predominantly people between 20 and 25 years of age are affected by the viral disease in the genital and anal area. The human papillomaviruses (HPV) that cause condylomata increase the risk of cervical cancer in women.
Symptoms: Recognizable by small, soft, painless, pink warts on the foreskin, urethra, penile shaft, or anus. In women, the warts also appear on the labia and at the vaginal entrance.
Infection: Genital warts are usually triggered by so-called human papilloma viruses (HPV), which are usually transmitted during unprotected sexual intercourse.
Treatment: "There is a simple, painless way to treat genital warts, and that is with an ointment containing the active ingredient imiquimod. It strengthens the local defenses. It needs to be applied only 3 times a week, does not cause redness and burning, is more effective than previous methods," explains Professor Karatepe. Alternatives: liquid nitrogen, laser and surgery.
Common STD #6: Herpes
It is one of the most commonly transmitted infectious diseases worldwide.
Symptoms: Type I herpes (formerly known as labialis) usually occurs on the lips, while type II (genitalis) occurs in the intimate area. "Today we know that both types of herpes can also occur in both places," explains Dr. Eva Thoma-Greber. The symptoms are also the same: small blisters and a burning and stinging pain in the affected areas. In the genital area, the blisters are often rubbed open very quickly.
Infection: According to estimates, up to 90% of the population is infected with herpes. In some, the disease never breaks out, in others it recurs. Infection occurs through skin contact with the acutely infected areas. Condoms do not provide reliable protection. Infection via glasses or cutlery cannot be completely ruled out.
Treatment: In the case of limited cold sores, it is often sufficient to apply a disinfecting ointment or one containing the active ingredient aciclovir. In the case of frequent or more extensive outbreaks, the substance must be applied internally. In addition, the affected region is treated antiseptically to prevent a secondary bacterial infection. If it catches you, you should - as with any sexually transmitted disease, by the way - ask the doctor to check for other STDs, if he does not suggest it himself anyway. The rule among experts is that one rarely comes alone.
Anything else? You can never get rid of herpes viruses completely; whenever your immune system is down, the blisters can come back. Sometimes a sunburn is enough. As soon as the characteristic tingling appears, kissing and sex are forbidden, even with condoms.
Common STD #7: Gonorrhea (also: gonorrhea).
Gonorrhea is considered extremely contagious. According to estimates, 60 million people worldwide become infected with the pathogen every year - men and women alike.
Symptoms: 2 to 5 days after infection with gonococci, a yellow-white fluid drips from the penis and it burns when peeing. Purulent discharge may also occur in women, but this is often less noticeable. If left untreated, this fluor disappears after a few weeks, and the infection "rises" and affects the prostate and epididymis in men. Then gonorrhea is difficult to diagnose. One can also become infected anally as well as orally. In the case of anal gonorrhea, the symptoms are not very typical; in many cases, eczema is suspected at first. In oral gonorrhea, the affected person hardly notices anything, but it is still contagious.

Infection: Through intimate contact. Condoms provide reliable protection. Infection via shared towels or toilet seats is extremely rare, but conceivable.
Treatment: If gonorrhea is suspected, a smear test is taken. In the uncomplicated early form, a single dose of antibiotics is usually sufficient.
What else? Stay abstinent until cured and inform your sexual partners. You should also have a check-up after four to ten days, because the pathogens can be resistant to the medication.
Common STD #8: Hepatitis B
Around 5 to 8% of Germans have already contracted liver inflammation triggered by the hepatitis B virus. In every tenth person affected, the infection develops into a chronic disease.
Symptoms: Flu-like signs appear no later than 6 months after infection. Signs of hepatitis include headache, aching limbs, fever, fatigue, diarrhea, loss of appetite, and jaundice.
Infection: Hepatitis viruses are found in all body fluids exchanged during sex.
Treatment: In most cases, the disease heals on its own. Doctors usually prescribe bed rest. Chronic infections are treated with medication.
Anything else? Vaccination offers real protection against hepatitis infection.
Common STD #9: Aids / HIV
The immunodeficiency disease Aids (Acquired Immune Deficiency Syndrome) is the most dangerous sexually transmitted infectious disease.
Symptoms: 3 to 8 weeks after infection, fever, diarrhea, skin rashes, flu-like symptoms and also swelling of the lymph nodes can occur. The actual disease does not break out until years later. Then the immune system is weakened by the HI virus to such an extent that infections of all kinds as well as certain types of cancer such as Kaposi's sarcoma have an easy time. The first sign is often a fungal disease of the mouth (thrush).
Infection: Through vaginal fluid, semen, blood. Condoms protect against HIV. The most dangerous is unprotected anal sex, because this often results in small injuries through which the virus can enter the body. Oral sex is also not harmless and can lead to AIDS. Infection is not possible during kissing or through shared cutlery, but it is possible through infected sex toys, razor blades and medical instruments.
Not dangerous: the bite of a mosquito that has previously sucked on an infected person. "The virus cannot reproduce in mosquito cells because they lack the appropriate receptor," says Professor Lutz Gürtler of the University of Greifswald. "The amount of blood adhering to the biting proboscis is not sufficient for infection."
Treatment: Antibodies can be detected in the blood from the second week after infection. An infection can only be ruled out with certainty after 3 months. The test is repeated to exclude false diagnoses. Those who are HIV-positive can start taking medication immediately, but they don't have to. "It depends on the patient's condition," Thoma-Greber says. To assess this, the doctor determines the viral load and the number of CD4 cells in the blood at least every 3 months. These are the immune cells that are destroyed by the HI viruses. The therapy always includes 3 or 4 preparations that keep the viruses in check. Which combination is chosen depends on how the patient tolerates it and whether it works for him. The tablets must be taken at exactly the right time (every 8 to 12 hours) - otherwise the concentration of active ingredient is too low at times, and the pathogens can become resistant.
A Harvard study among AIDS researchers caused quite a stir. According to this study, the immune system seemed to be able to keep the viruses in check on its own if the patients received highly active antiviral treatment (HAART) within the first 180 days after infection. However, the result is not yet considered fully confirmed.

Anything else? "If one has been exposed to HI viruses, taking medication immediately seems to significantly reduce the risk of infection. This is indicated by experiences with medical personnel, for example, when someone had cut themselves with a contaminated medical instrument," says Thoma-Greber. Anyone who has an infected partner should ask their doctor about post-exposure prophylaxis (PEP) - in case a condom breaks, for example. But: The mere fear after a one-night stand is not enough for a prescription. Besides, the whole thing also has serious side effects.
How can I protect myself from STDs?
The most reliable way to protect yourself against STDs is to keep the change of sex partners to a minimum. A condom protects against pathogens every time you have sex. Good intimate hygiene can reduce the risk of smear infections. You can get vaccinated against hepatitis A and B and human papillomavirus (HPV). If you recognize warts or blisters on a partner, avoid sexual contact - including oral sex!
Have I been infected?
Because the symptoms of a sexually transmitted infection are often difficult to recognize and even disappear after a few days after infection, although the infection is still there, it is advisable to go to a doctor immediately at the slightest sign. Then you do not risk subsequent damage and infection of others. In the best case, go to a doctor for skin and sexually transmitted diseases or a urologist. Women can also visit a gynecologist. In addition, it is possible to be tested anonymously for an STI at many health offices.
These symptoms are suspicious
If you have the following complaints, you should not wait any longer and see the doctor:
Burning when urinating
Skin changes such as warts, blisters, or a rash
itching in the genital area and anus
unusual white or unpleasant-smelling discharge from the penis or anus
pain in the lower abdomen, penis or testicles
Sometimes general signs of illness such as fever, swollen lymph nodes, fatigue, sore throat and loss of appetite accompany the infection.
How does the doctor examine you?
The examination at the doctor's is not bad and is done routinely by the specialist. The main diagnostic procedures are:
Blood examination
Urine examination
Swab of vagina, urethra, throat or buttocks
Visual diagnosis
Health insurance companies usually cover the costs if there are symptoms or a concrete suspicion of an STI - even if the partner is known to have a sexually transmitted disease.
Conclusion: Never forget condoms!
It can't be said often enough: to protect yourself from STDs, you should wear a condom at all times. If you have frequently changing sex partners, you should be even more careful about contraception and hygiene. At the slightest sign of infection, go to the doctor immediately to protect yourself and your partner.






Comments
There are no comments for this story
Be the first to respond and start the conversation.