Understanding the Impact of COVID-19 on the Brain
Neurological Complications in Acute COVID-19
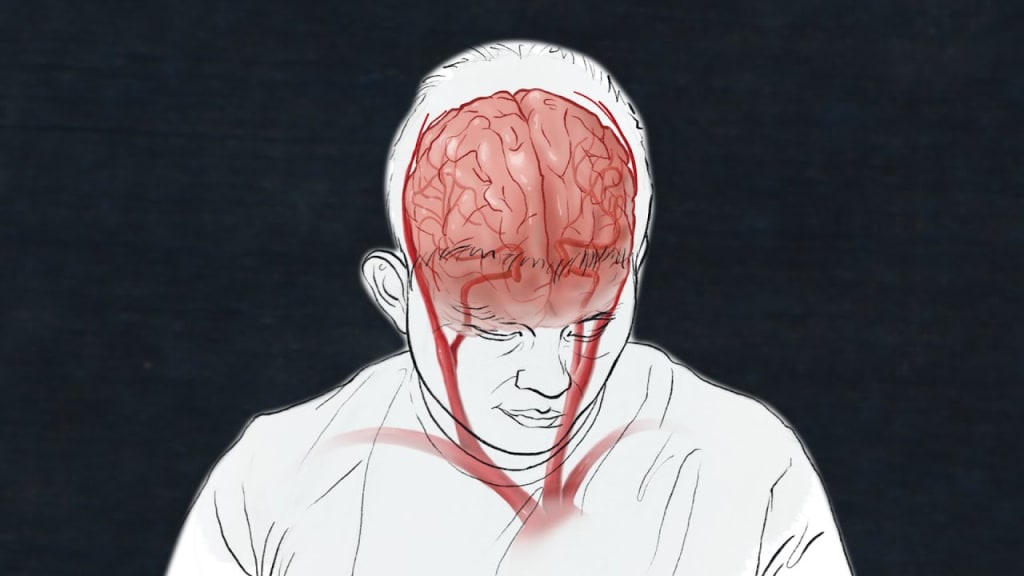
Since the emergence of the COVID-19 pandemic, much attention has been focused on its effects on the respiratory system. However, as the pandemic has unfolded, it has become increasingly clear that the virus, known as SARS-CoV-2, can have profound impacts on various parts of the body, including the brain. In this article, we will delve into the neurological complications associated with COVID-19, both in acute cases and among those with long-lasting symptoms, often referred to as "long COVID." We will explore the underlying mechanisms, potential treatments, and the broader implications of this research.
Neurological Complications in Acute COVID-19
The Brain's Vulnerability
From the early stages of the pandemic, scientists anticipated the possibility of neurological complications. Drawing on past experiences with viral pandemics, such as HIV/AIDS, which also exhibited long-term cognitive problems, it was clear that the brain could be a target for SARS-CoV-2. The consequences of brain involvement in a viral infection can be devastating, affecting personality, cognitive abilities, mood, and overall well-being.
Autopsies Reveal Brain Damage
Autopsies of individuals who succumbed to COVID-19 have unveiled alarming evidence of brain damage. The findings included damaged blood vessels, the presence of inflammatory cells surrounding the brain, and antibodies adhering to blood vessel walls. Surprisingly, despite the virus's impact on the respiratory tract, researchers did not find substantial amounts of the virus in the brain itself. Although some reports mention minuscule viral quantities, they fail to account for the observed brain pathology.
Long COVID and Brain Symptoms
The Enigma of Long COVID
While the neurological complications in acute cases are concerning, a more perplexing aspect of the virus is its long-term effects on the brain. Long COVID, characterized by persistent symptoms lasting weeks or even months after the initial infection, presents a unique challenge. Studies suggest that up to 30% of COVID-19 survivors may develop long COVID, with women at a higher risk.
Diverse Neurological Symptoms
Long COVID patients experience a range of neurological symptoms, falling into several categories. These include:
Brain Fog: Patients often report cognitive difficulties, such as poor concentration and memory problems.
Skin Changes: Some describe abnormal sensations on their skin.
Headaches: Chronic headaches are a common complaint.
Psychiatric Symptoms: In rare cases, individuals may experience severe delusions or psychosis.
Diagnostic Challenges
One of the major difficulties in diagnosing long COVID-related brain issues is that conventional tests often yield negative results. Even MRI scans, known for their sensitivity in detecting brain changes, may appear normal. Researchers have resorted to more specialized tools to evaluate immune system functioning and subtle neuronal injuries that standard scans may miss.
Investigating the Mechanisms
Three Hypotheses
Researchers are exploring three hypotheses to explain how long COVID affects the brain:
Direct Viral Infection: SARS-CoV-2 might infect specific brain cells or supportive structures.
Autoimmune Response: Autoimmune reactions may target brain components, leading to various symptoms.
Distal Inflammation: Inflammation in other parts of the body, like the lungs, could trigger lasting changes in brain cells.
It's possible that a combination of these mechanisms or a sequential occurrence of events contributes to the neurological issues observed in long COVID.
Potential Treatments and Rehabilitation
Autonomic Rehabilitation
To address the neurological symptoms of long COVID, rehabilitation techniques have been developed. Autonomic rehabilitation, in particular, focuses on restoring balance to the autonomic nervous system. This approach involves gentle movements and breathwork to increase blood flow into the chest cavity, improving symptoms such as brain fog and dysautonomia.
Drug Trials
Researchers are also exploring drug treatments to target the root causes of long COVID. Some trials involve immune-modulating drugs, such as intravenous immunoglobulin and corticosteroids, which aim to modulate the immune response. However, these approaches are broad and affect the immune system in various ways, making precision challenging.
Vaccination as a Hope
Vaccination has shown promise in alleviating long COVID symptoms for some individuals. It may eliminate persistent virus remnants triggering chronic inflammation. However, not everyone benefits equally from vaccination, as it can exacerbate autoimmune diseases in some cases. The challenge lies in identifying what triggers symptom improvement to develop alternative therapies.
Implications and Future Research
The knowledge gained from studying long COVID extends beyond this specific disease. Millions of people suffering from post-viral illnesses, like post-Lyme syndrome and Gulf War syndrome, may benefit from the insights gained. By applying the best available tools and research, there is hope that these conditions, which have long baffled medical professionals, can be better understood and treated effectively.
In conclusion, while COVID-19's impact on the respiratory system is well-documented, its effects on the brain, both in acute cases and in the long term, are an evolving area of research. Understanding these neurological complications is crucial not only for current patients but also for addressing similar challenges in the future.





Comments
There are no comments for this story
Be the first to respond and start the conversation.