Vascular Compression Misconceptions (part 4/4)
Separating Fact from Fiction

Welcome back for the final part of our blog post series focusing on vascular compression diseases (VCDs), where we debunk prevalent myths and misconceptions. If you're just joining us and haven't yet delved into the previous parts of this series, you can catch up by exploring part 1, part 2, and part 3. In this concluding chapter, we persist in our mission to eradicate misconceptions and shed light on the truth.
Misconception #16: Symptoms are always severe
Fact: The severity of symptoms associated with VCDs can vary greatly from person to person and may even fluctuate in intensity for an individual over time. Some people may experience severe or debilitating symptoms, while others may have mild or manageable manifestations. It is essential to recognize that the presence and severity of symptoms can differ among individuals with the same condition, and timely diagnosis and treatment are crucial for managing symptoms and preventing complications.
Gradual onset - Compressive disorders that develop slowly over time allow for gradual accommodation and collateral circulation to become established, minimizing acute symptom severity. Tenderness, aching and fatigue may emerge before sharp or intense pain, raising awareness early on. Examples include age-related degenerative stenosis or repetitive overuse conditions.
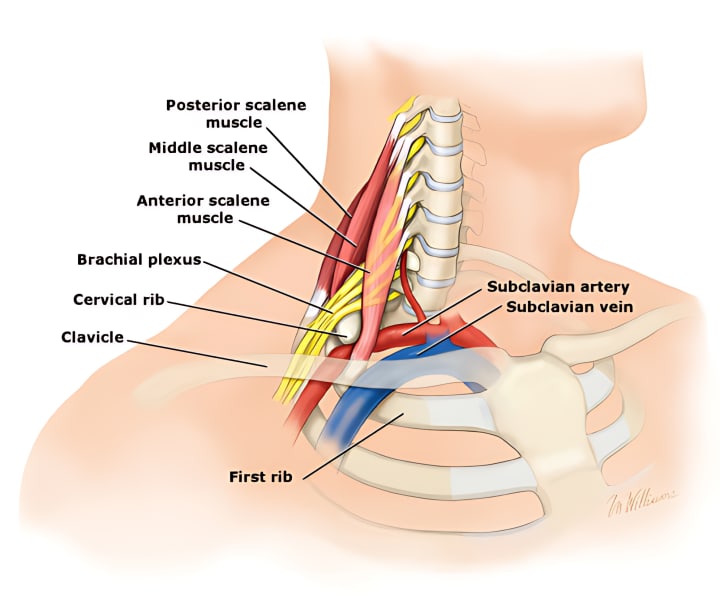
Intermittent symptoms - Dynamic compressions which occur only with certain postures or during specific activities produce symptoms that come and go, rather than being constant. Changing position or eliminating the provoking activity relieves discomfort, limiting severity and life disruption. Neurogenic thoracic outlet syndrome and median arcuate ligament syndrome often follow this pattern.
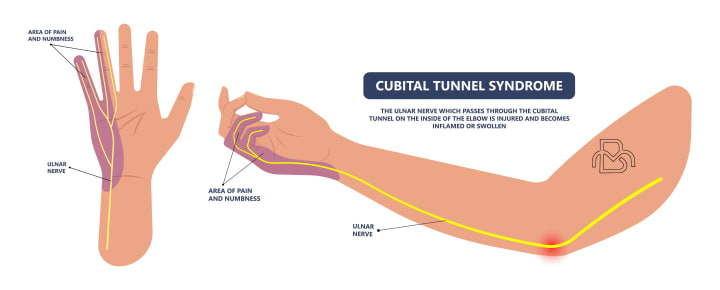
Sensory only - Impingement of sensory nerves alone results in numbness, tingling and sensitivity rather than pain. Motor and circulatory function remain intact. Disability may be negligible with altered sensation alone, allowing normal activity to continue. Some ulnar neuropathies at the elbow follow this profile.
Adaptability - Cervical ribs, anomalous muscles and small thoracic outlets present from birth but remain asymptomatic for some due to individual adaptability. As surrounding tissues accommodate to the abnormality over years, symptoms may never arise or emerge only during times of musculoskeletal strain, allowing minimal discomfort relative to the underlying compression. Surgical intervention becomes optional.
Inflammation - Chronic nerve and vessel irritation trigger inflammation with swelling that tends to flare and then subside over the course of days to weeks. During dormant periods between acute flare-ups, baseline discomfort remains limited as long as activities that provoke inflammation are avoided. Ongoing management with rest, physical therapy, etc. aims to extend time between flare-ups by controlling inflammation.
Distensibility - Laxity of nearby connective tissue creates more space to accommodate compressed structures, limiting severity until late stages. Some degree of venous insufficiency provides venous flow through alternative channels. Stenotic lesions of the celiac axis and mesenteric arteries in some patients remain asymptomatic due to extensive collateral branches that form over time from chronic ischemia.
Central adaptation - The central nervous system may become desensitized over time to ongoing compression from certain disorders like cervical stenosis or thoracic outlet syndrome, raising pain tolerance and limiting perceived severity and disability. While risks associated with the anatomical compression remain, quality of life is upheld through this adapted state as long as symptoms continue to gradually decline or stabilize.
So the level of severity and life disruption experienced from any VCDs depends on a variety of patient-specific factors in addition to the nature of the anatomical disorder itself. The pace of development, activity triggers, sensory components, adaptability and inflammatory mechanisms involved for each individual, combined with their pain tolerance and psychological state, ultimately determine symptom intensity and the degree of disability perceived - which may range from negligible to profound.
Conditions prone to gradual onset with intermittent or sensory-only symptoms and a capacity for adaptation typically allow the most latitude for conservative management and accommodation. But duration and progression must be monitored, as severity will increase over time without treatment for most compressive lesions. Accurate expectation and education help patients understand how symptoms may be limited or stabilized to a tolerable level with proper self-management in some cases, avoiding premature pursuit of aggressive treatments unless significant deterioration occurs.
Each patient experiences and reacts to a vascular compression uniquely based on physical as well as cognitive factors. So while presumed that severe or debilitating symptoms would be ubiquitous, the reality and clinical picture for any individual may vary widely within the range of what is known and possible for their particular condition based on its usual presentation. A full understanding of a patient's experience requires insight into not only the anatomical pathology involved but also their own adaptability, sensitivity, attitude and circumstances. Perceived severity alone should not dictate management without consideration of all contributors. Significant improvement relies not just upon resolution of the underlying compression but also modifications addressing these additional influences to the extent possible through collaborative efforts.
Misconception #17: Effective treatment will cure the underlying condition
Fact: While treatment for VCDs can often lead to significant symptom improvement and restoration of function, it is important to recognize that not all cases will result in a complete cure of the underlying condition. The goal of treatment is typically to alleviate symptoms, improve function, and prevent complications, but some individuals may continue to experience residual symptoms or require ongoing management even after successful treatment. It is unrealistic to expect that any treatment for a chronic VCD will necessarily provide a permanent "cure" or eliminate the underlying anatomical impairment and predisposition to recurrence in all cases. While treatment aims to relieve current symptoms and disability by eliminating or alleviating the factors directly responsible for nerve and vessel entrapment at a given point in time, the potential for re-development of compression persists life-long in the majority of patients. Effective management impacts symptoms, not inherent susceptibility.
There are several reasons why vascular compressions cannot be cured outright in most circumstances:
Fixed structural abnormalities - Options such as surgery can correct compressive lesions like cervical ribs, small thoracic outlets or median arcuate ligament syndromes, however the surrounding tissues remain at risk of again narrowing over time with new bone spur formation or soft tissue contracture. Revision procedures may eventually be required, though risk is often years away.
Muscle tension and spasms - Procedures to release muscles prone to spasm and entrapment such as scalenectomy may weaken or remove the muscles, but without maintenance the remaining muscles may tighten to again compress nerves and vessels, re-establishing symptoms. Ongoing physical therapy and postural training is key to prevention.
Poor posture and flexibility - Though postural correction and targeted exercise may temporarily relieve compressive symptoms, habitually poor posture and chronic inflexibility place tension on areas like the thoracic outlet and celiac plexus which readily recurs without motivation and persistence in proper positioning and range of motion. Continued discipline is mandatory to avoid re-compression.
Underlying inflammation - While rest, medication, physical therapy and nerve blocks may calm symptomatic inflammation in compressed locations, the inflammatory response has not been eliminated. Repetitive use or injury at these sites readily provokes new flare-ups, requiring ongoing management and modification to contain. An anatomical predisposition to inflammation still exists.
Central sensitization - Once the central nervous system has become sensitized to chronic compression, changes do not readily reverse even when an initial anatomical issue has been resolved or inflammation calmed. Persistent pain may continue from heightened sensitivity until gradually extinguished over time with desensitization treatments. Early intervention is most effective at limiting development of central sensitization.
Scarring and adhesions - Surgical and minimally invasive decompression procedures necessarily cut through and disrupt normal tissues. Though the primary compression has been relieved, scarring forms within surrounding areas which have the potential to limit function and again entrap nerves and vessels to some degree. Time, physical therapy, and revision surgery may eventually address, but do not cure this tendency.
So, while there are many effective ways to relieve the signs and symptoms of most VCDs through both surgical and non-surgical means, a permanent cure that eliminates the potential for any recurrence or new development of compression is typically not realistic given the nature of the predisposing factors involved. Patients must remain vigilant with precautions and maintenance strategies specific to their condition to extend symptom-free periods and minimize risks of re-compression and disability.
A "cure" for any chronic medical condition suggests a permanent elimination of health risks and consequences with return to a normal disease-free state, which for most is not the outcome that can be expected from treatment for vascular compression disorders alone given the dynamics involved. While highly effective at relieving current impairment, these interventions do not typically reset patients to a pre-disease baseline or remove their inherent propensity which mandates subsequent avoidance and management. Treatment impacts the symptom, not the susceptibility. An understanding and acceptance of this reality is important to maintaining both health and quality of life.
Misconception #18: Recovery from treatment takes a long time
Fact: The recovery time following treatment for a VCD can vary widely, depending on the specific condition, the severity of the compression, the type of treatment, and the individual patient's health status. In some cases, patients may experience significant symptom relief and return to normal activities relatively quickly, while in others, recovery may take longer or require additional rehabilitation.
Some reasons why recovery from certain vascular compression treatments may proceed rapidly include:
Conservative management - Options such as rest, physical therapy, massage, medication, and nerve blocks aim to relieve symptoms without correcting underlying anatomical abnormalities. By reducing inflammation, muscle spasms and pain through conservative means, significant improvement can occur within weeks allowing return to normal or modified activity. Residual symptoms are still possible, but quality of life may be restored.
Minimally invasive procedures - Techniques like botox injections, venography with angioplasty or endovascular stent placement help alleviate compression through small punctures without the need for open surgery. Recovery requires limited downtime with most patients resuming light activity within days or weeks, experiencing near complete resolution of symptoms. Risks of bleeding, stiffness and disability are minimized.
Targeted muscle release - Procedures such as pectoralis minor tenotomy, scalene muscle release or celiac plexus block and neurolysis specifically sever or weaken muscles responsible for compression in some cases. By precisely interrupting the source of nerve/vessel entrapment through minor surgery, symptoms improve quickly while sparing nearby tissues. Early physical therapy optimizes outcome, but prolonged inactivity is usually unnecessary.
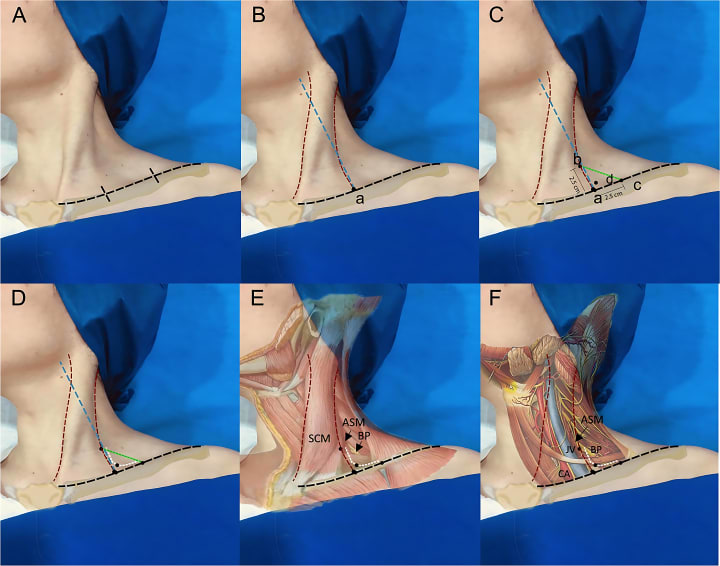
Thoracic outlet decompression - Transaxillary first rib resection, cervical rib excision or soft tissue procedures to open the thoracic outlet provide rapid relief of neurogenic and venous symptoms by restoring space and mobility. With a minimally invasive surgical approach, the majority of patients return to work and light activity within a month, with full recovery within 2 to 3 months. Disability is typically limited as surrounding structures remain untouched.
Postural rehabilitation - For select patients, a course of physical therapy and postural training may adequately relieve compressive symptoms from conditions such as mild thoracic outlet syndrome or median arcuate ligament syndrome without other intervention. By learning proper shoulder, chest and spine positioning and flexibility through guided exercise, decompressive effects may become apparent within a month, though ongoing discipline is required to prevent recurrence.
With tailored and minimally invasive treatments now available for certain compressive disorders, prolonged recovery periods are often avoidable. Each patient must be evaluated based on the specifics of their condition to determine the optimal approach most likely to provide safe and swift relief with limited impact. An open mind regarding innovative options and a willingness to modify activity levels during healing and rehab can aid rapid recovery where procedures themselves are uncomplicated. When facing a VCD, extended periods of disability are not an absolute.
Misconception #19: vascular compression diseases are always caused by a blood clot
Fact: Although blood clots can lead to VCD in some cases, not all vascular compression syndromes are caused by blood clots. Vascular compression diseases can result from various factors, including anatomical abnormalities, muscle imbalances, inflammation, and repetitive stress. It is important to consider the diverse range of potential causes when evaluating a patient with a suspected VCD.
Accurately identifying the underlying cause of symptoms in each case allows for targeted and effective treatment to relieve compression with minimal risk of recurrence. Though rarely implicated, blood clots when present must also be addressed through anticoagulation and clot removal to restore circulatory function in addition to correcting any associated anatomical or muscular problems. VCDs are diverse, with no single causative factor responsible for all cases, including thrombosis alone.
Misconception #20: Vascular compression syndromes can be treated with home remedies
Fact: Certain home remedies may potentially relieve symptoms temporarily. For example, exercises that aim to improve posture, strengthen muscles, or promote blood flow may help alleviate some discomfort associated with these conditions. Similarly, lifestyle modifications, like adopting a healthy diet and maintaining a balanced weight, can potentially help manage the symptoms. However, it's crucial to understand that these home remedies are not definitive treatments for VCDs. They may help manage the symptoms, but they don't address the underlying issue: the physical compression of the blood vessels or nerves.
The main treatments for VCDs are surgery or minimally invasive vascular procedures. Surgery can decompress the area by altering anatomy and creating more space. Minimally invasive vascular procedures, like vein stenting in May-Thurner syndrome, use devices inserted through small incisions to open up the compressed blood vessel. VCDs will not improve on their own, and home treatments do not fix the underlying problem. Symptoms may even worsen over time if the compression is not corrected. Appropriate diagnosis and treatment from a doctor are essential to properly treat VCDs.
In conclusion, it's evident that vascular compression syndromes are surrounded by numerous misconceptions, many of which we've dissected in our previous posts. From misunderstanding the nature of the symptoms, to over-simplifying the complexity of diagnosis and treatment, these misconceptions can lead to delays in treatment and unnecessary suffering. The reality is that these syndromes are complex, can affect people differently, and require an individualized and holistic approach for diagnosis and management. As we continue to deepen our understanding of these conditions, we must strive to debunk these misconceptions, promote accurate information, and ensure that patients receive the right diagnosis and treatment at the right time. Let's continue the conversation, dispelling myths, and spreading awareness about vascular compression syndromes.
About the Creator
Mohammad Barbati
Mohammad E. Barbati, MD, FEBVS, is a consultant vascular and endovascular surgeon at University Hospital RWTH Aachen. To date, he has authored several scientific publications and books regarding vascular and venous diseases.






Comments
There are no comments for this story
Be the first to respond and start the conversation.