Vascular Compression Misconceptions (part 3/4)
Separating Fact from Fiction
Greetings once again! This is the third part in our series tackling the common misconceptions surrounding vascular compression diseases (VCDs). If you haven't had the chance to read previous posts, feel free to check it out (part 1 & part 2). In this post, we continue our journey of debunking myths, and dispel some falsehoods.
Misconception #11: Vascular compressions diseases are always caused by a structural abnormality
Fact: It is an oversimplification to conclude that all VCDs result from a clearly defined anatomical abnormality. While structural narrowings such as a small thoracic outlet, cervical rib or vascular anomaly are implicated in some cases, other factors including muscle tension, inflammation and nerve hypersensitivity may also play a significant role in symptoms for certain patients. A structural compression is not required for a compression syndrome to occur or persist in every case.
They can lead to tissue damage. Compression of arteries and veins reduces blood flow to tissues. This lack of blood flow deprives tissues of oxygen and nutrients, which can cause tissue damage and even tissue death. For example, compression of arteries in the legs is a common cause of gangrene.

They can lead to aneurysms. Compression and distortion of blood vessels over time can cause abnormal dilation or bulging of the vessel called an aneurysm. Aneurysms have a high risk of rupturing and leading to severe internal bleeding.
They can be life-threatening. Compression of certain major blood vessels, such as the aorta or carotids, can severely impact blood flow. A sudden blockage of these critical vessels can lead to stroke, organ damage, or death.
They often get worse over time. Vascular compressions tend to be progressive diseases. Just because symptoms are mild initially, does not mean they will stay that way without treatment.
Misconception #13: Vascular compressions diseases always improve with rest
Fact: While rest can be an essential component of the treatment plan for some VCDs, it is not a universal solution for all cases. In fact, prolonged rest or immobilization can sometimes exacerbate symptoms or lead to complications in certain conditions. The appropriate treatment approach depends on the specific VCD, the underlying cause, and the individual patient's needs. It should also be noted that inflammation from compression may continue even at rest. Swelling around compressed areas can persist and continue to cause pain, numbness or impaired circulation without treatment. Resolution of inflammation may require medical therapies in addition to rest.
Or, muscle spasms and poor posture are not corrected with rest. For some patients, muscle tightness, spasms or postural issues contribute to compression. Physical therapy and non-surgical interventions are typically needed to properly address these issues. Rest alone will not rehabilitate muscles or correct posture.
For example, Thoracic Outlet Syndrome (TOS) can be caused by structural abnormalities like the presence of an extra cervical rib or an anomalously narrow thoracic outlet. However, TOS can also result from functional factors such as poor posture, muscle imbalances, or repetitive strain from activities that involve the upper extremities.
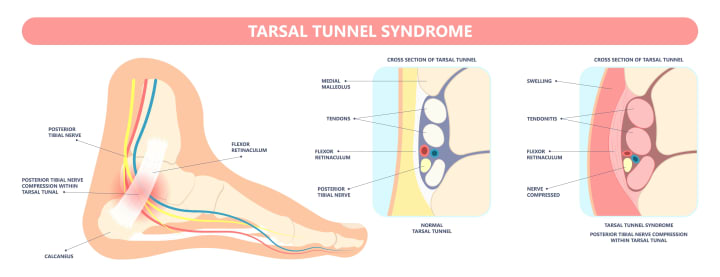
Similarly, Tarsal Tunnel Syndrome, a compression neuropathy of the posterior tibial nerve, can be caused by structural issues like a bone spur or a ganglion cyst, but it can also result from functional factors such as inflammation, muscle imbalances, or overuse.
So, while a short period of rest can be useful in managing flare-ups of symptoms from vascular compression diseases, significant and lasting relief will usually require treatment of the underlying anatomical compression and any other contributory factors like muscle tightness or poor posture. Complete recovery without intervention directed at the source compression issue is unlikely for most patients. Rest should only be viewed as a temporary palliative measure until proper diagnosis and treatment is established. Compression disorders often will not adequately or permanently improve without appropriate medical therapy, physical therapy, medication, or procedure depending on the condition and severity.
Misconception #14: Vascular compressions diseases are always caused by an injury
Fact: Although injuries can contribute to the development of some VCDs, these conditions can also result from congenital anatomical abnormalities, age-related changes, or other factors unrelated to trauma. It is essential to recognize the diverse array of underlying causes in order to accurately diagnose and effectively treat VCDs.
Non-traumatic factors commonly linked to vascular and neurogenic compressions include:
Repetitive arm movements - Jobs, hobbies or activities requiring excessive overhead arm use or movements can place tension and stress on the brachial plexus, subclavian vessels and surrounding muscles. Over time, this repetitive stress may narrow passageways or provoke muscle spasms resulting in compression symptoms. Reducing inciting arm activity is often an integral part of management.
Poor posture - Slouched or rounded shoulder posture, forward head position and pectoralis minor tightness pull the neck, shoulders and upper chest out of alignment. This postural strain can directly compress nerves and vessels of the neck and upper limb or lead to muscle spasms that entrap these structures. Posture correction is essential to treatment.
Congenital anomalies - Some individuals are born with abnormalities such as cervical ribs, extra scalene muscles or a rigidly narrow thoracic outlet that make them prone to developing compressions, especially with age. Surgical correction of the anomaly may be required in severe cases.
Degenerative changes - Age-related degeneration of the cervical and upper thoracic spine often includes loss of disc height, bone spur formation and joint enlargement. These changes can narrow the spaces through which arteries, veins and nerves travel, resulting in gradually progressive compression and symptoms. Conservative and minimally invasive options are typically pursued before spinal surgery for this group.
Tumors - The growth of tumors in vicinity of the brachial plexus, subclavian vessels or thoracic outlet can occupy space and directly compress surrounding structures. Benign tumors may be monitored if asymptomatic but may require excision if causing substantial compression resulting in pain, weakness or circulatory changes.
Inflammation - Conditions like thoracic outlet syndrome and median arcuate ligament syndrome are linked to chronic inflammation in and around compressed areas such as the scalene triangle and celiac artery, respectively. Reducing inflammation through rest, physical therapy, medications and nerve blocks is key to relieving compressive symptoms, especially during acute flare-ups of pain or exacerbation from activity. An underlying anatomical narrowing may still need to be addressed for lasting benefit.
So while injury can be one precursor for certain vascular and neurogenic compressions, most cases involve gradual development over time due to repetitive overuse, poor posture, congenital predisposition, degenerative changes or chronic inflammation. A detailed history often reveals these non-traumatic factors, which must be addressed to achieve optimal management of symptoms in addition to any interventions directed at the anatomical compression itself. Significant compressions that arise solely or directly due to an injury usually present with acute and severe disability requiring immediate medical attention.
For most patients with VCDs, proper diagnosis and treatment includes correcting any non-traumatic causes or contributors to the condition in combination with relieving the compression through physical therapy, nerve/muscle procedures or surgical decompression when needed. An integrated approach provides the greatest likelihood of success and minimizes risk of recurrence by resolving all underlying issues, not just a single traumatic event. While injury may be a precipitating factor in some cases, most compressive syndromes develop due to repetitive stress, poor posture, inflammation and degeneration. Comprehensive management should focus on all potential causative and aggravating influences.
Misconception #15: Exercise and activity should be avoided
Fact: Contrary to the misconception that exercise, and activity should be avoided in individuals with VCDs, engaging in regular physical activity can be beneficial in many cases. Exercise can help maintain muscle strength, improve posture, and support overall cardiovascular health. It is important, however, to choose appropriate activities and ensure that they are performed with proper technique and form to avoid exacerbating symptoms or causing further injury.
Of course, some activities may need to be modified or avoided, depending on the specific condition and its severity. For example, individuals with TOS may need to avoid activities that involve repetitive overhead arm movements or heavy lifting, as these actions can exacerbate symptoms. Similarly, patients with lower extremity VCDs may need to avoid high-impact activities that place excessive strain on the affected leg.
Some reasons why total avoidance of activity is not recommended for VCDs include:
Muscle atrophy - Immobility causes muscles to weaken and waste away, including those required to support areas of compression and maintain proper posture. Strong, flexible muscles are needed to stabilize vulnerable regions and prevent re-compression. Targeted exercise builds muscle to relieve and prevent symptoms.

Poor flexibility - Lack of motion allows connective tissues to tighten, limiting range of motion in the neck, shoulders, chest and back. Stiffness itself stresses compressed passages and predisposes to new flare-ups. Controlled stretching and mobility exercises maintain extensibility of these regions.
Weak core muscles - The torso muscles support the spine, ribs and shoulders. Weak core muscles cannot properly hold the upper body in alignment, allowing slouching and rounding that compresses nerves and vessels. Core strengthening helps sustain an upright, neutral posture.

Weakened bones - Disuse osteoporosis develops from lack of weight-bearing activity. Bone loss provides less protection and anchorage for muscles and connective tissue, allowing slackening and drop of the shoulder girdle which tensions the brachial plexus. Impact exercise such as walking prevents the decline in bone density that would otherwise hasten compression.

Central sensitization - Prolonged inactivity due to pain leads to increased perception of and focus on discomfort as well as other psychological effects. Light activity such as leisure walking raises pain tolerance while also improving mood and motivation. In moderation, it helps overcome sensitization and the tendency toward excessive rest.

Reduced circulation - Lack of activity impairs venous return and lymphatic drainage from the arms, exacerbating or prolonging swelling in compressed areas. Low-level exercise such as shoulder rolls, arm swings and flexing/extending wrists and fingers enhances circulation to speed healing and reduce risk of blood clots or scarring post-procedure.
Weight gain - A sedentary lifestyle predisposes to weight gain which places extra load on the shoulders, neck and chest, worsening any tendency toward compression. Losing excess pounds through modified diet and exercise lightens the burden on at-risk areas. Exercise also raises metabolism to help sustain weight loss.
So prescribed activity and targeted exercise are not only safe but vital to recovery and prevention of recurrent vascular compression. Prolonged rest alone leads to muscle atrophy, joint stiffness, poor posture, weight gain and psychological impacts that worsen prognosis. While high intensity, repetitive or overhead activity that provokes symptoms should be avoided, controlled upper and lower body exercise provides substantial benefits.
Light aerobic exercise such as walking combined with gentle stretching, postural training and targeted muscle strengthening should commence once significant pain and inflammation have resolved, usually within days to weeks of treatment. An individualized activity plan based on the location and severity of a patient's compressive disorder helps build strength and flexibility while avoiding re-injury. Significant improvements in pain, function and quality of life depend on restoration of normal motion and fitness, not enforced immobility.
About the Creator
Mohammad Barbati
Mohammad E. Barbati, MD, FEBVS, is a consultant vascular and endovascular surgeon at University Hospital RWTH Aachen. To date, he has authored several scientific publications and books regarding vascular and venous diseases.





Comments
There are no comments for this story
Be the first to respond and start the conversation.