Vascular Compression Misconceptions (part 1/4)
Separating Fact from Fiction
Imagine suffering from mysterious pain, numbness, weightloss or swelling that seems to come and go without explanation. For many people living with vascular compression diseases (VCD), this is their reality. And to make matters worse, these conditions are often misunderstood, leading to confusion, delayed diagnoses, and improper treatment. In this post (and next three posts), we'll dive into some of the most common misconceptions about VCDs, debunking myths and shedding light on the facts. From the severity of symptoms to the role of exercise in managing these conditions, we'll tackle the misunderstandings head-on to create a clearer picture for those affected and their loved ones. So sit back, and prepare to have your assumptions challenged as we unravel the truth behind these often-misunderstood ailments.
Misconception #1: Vascular compression diseases are rare
Fact: While VCDs are not as common as some other types of vascular conditions, they are not rare. In fact, it is estimated that up to 20% of the population may have some form of VCD. This means that millions of people around the world are affected by these conditions. VCDs occur when blood vessels or nerves become compressed, leading to a variety of symptoms and complications. The prevalence of these diseases varies greatly depending on the specific condition.
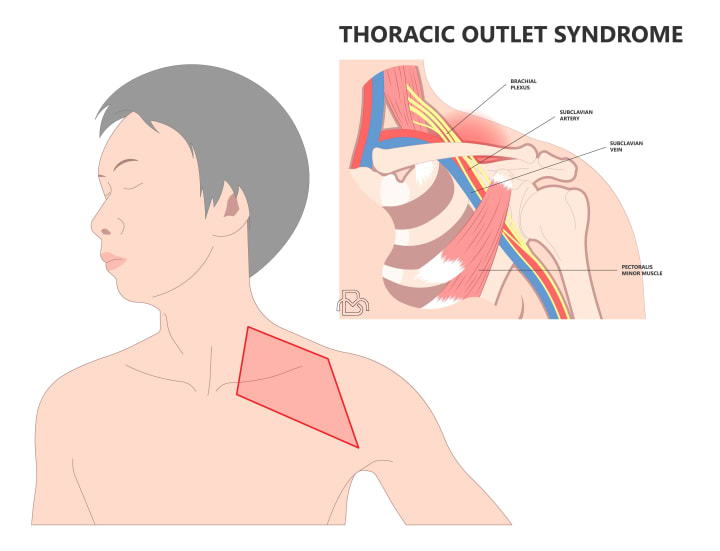
For example, Thoracic Outlet Syndrome (TOS) is a relatively common VCD that affects the nerves and blood vessels passing through the thoracic outlet, a narrow space between the collarbone and the first rib. It is estimated that TOS occurs in about 1 in 1,000 individuals, but this number may be higher due to underdiagnosis.
On the other hand, Nutcracker Syndrome, a VCD that involves the compression of the left renal vein, has an estimated prevalence of 0.1% to 2.5% in the general population. Understanding the true prevalence of these conditions is essential for medical professionals and researchers to develop appropriate diagnostic and treatment strategies.
Misconception #2: Vascular compression diseases only affect athletes or highly active individuals
Fact: Although some VCDs may be more prevalent among athletes or individuals who engage in intense physical activity, these conditions can affect all people, regardless of their activity level. VCDs are caused by a variety of factors, including anatomical abnormalities, injuries, and repetitive stress or strain on the affected area.
For example, Popliteal Artery Entrapment Syndrome (PAES), which involves the compression of the popliteal artery in the knee, is more common among athletes, particularly those who engage in sports involving repetitive knee flexion and extension. However, this condition can also occur in non-athletic individuals due to congenital abnormalities or previous trauma.

Similarly, Tarsal Tunnel Syndrome, a compression neuropathy of the posterior tibial nerve, can be caused by factors such as flat feet, obesity, or diabetes, which are not limited to athletes or highly active individuals. It is crucial to be aware that vascular compression diseases can affect people with various activity levels and lifestyles, and early diagnosis and treatment are essential for optimal outcomes.
Misconception #3: Surgery is always necessary to treat vascular compression diseases
Fact: This is a misconception that can lead to unnecessary or overly aggressive treatment. While surgery is sometimes required to treat certain VCDs, it is not always the first or only treatment option. The choice of treatment depends on the specific condition, the severity of the symptoms, and the patient's overall health. In many cases, non-surgical approaches such as physical therapy, pain management, and lifestyle modifications are initially recommended to alleviate symptoms and improve the patient's quality of life.
For instance, in cases of mild to moderate Thoracic Outlet Syndrome (TOS), conservative treatments like physical therapy, postural exercises, and pain management techniques are often sufficient to reduce symptoms and improve function. Only when these conservative measures fail, or when the patient's condition worsens, is surgery considered. Similarly, for some patients with May-Thurner Syndrome (compression of the left iliac vein by the right iliac artery), nonsurgical options such as anticoagulant medications and compression stockings may be effective in managing symptoms and preventing complications. However, more severe cases may require angioplasty with additional stenting. A thorough evaluation by a healthcare professional is crucial to determine the most appropriate course of treatment for each individual patient.
Misconception #4: Vascular compression diseases always show up on imaging tests
Fact: While imaging tests such as X-rays, MRI, CT scans, and ultrasound can be useful in diagnosing VCDs, they don't always provide a definitive diagnosis. Some cases of VCDs may present with subtle or transient changes that are not easily detectable on imaging studies. Additionally, the accuracy of imaging tests can be affected by factors such as the patient's body position, the imaging modality used, and the skill of the radiologist interpreting the results.
There are a few reasons why imaging may appear normal in some patients with vascular compression diseases:
1) Mild or intermittent compression may not always be captured, especially if imaging is only done in a static position rather than with provocative maneuvers. Dynamic compression may only occur with certain postures, movements or activities.
2) Imaging resolution may not be enough to detect subtle compressive lesions or abnormalities. As technology continues to improve, smaller compressions and anomalies are becoming more apparent. But some narrowings or impingements still may not be fully visualized.
3) Physical exam findings and symptoms may be caused by other factors like muscle spasms, inflammation or nerve sensitivity. So even when no compression is noted, patients may still benefit from treatment.
4) Vascular compressions may be more significant when surrounding tissues are swollen or inflamed. The compression visualized during a flare-up of symptoms may not be as severe once inflammation has resolved.
It is essential for healthcare providers to consider the patient's clinical presentation and history in addition to imaging results when making a diagnosis. Imaging may be normal for some, but symptoms may still warrant a trial of compression therapy to determine if there is evidence of improvement before ruling out a vascular compression syndrome.
Misconception #5: Medications do not work and are just meant to relieve pain
Fact: While some medications prescribed for VCDs may primarily focus on relieving pain, others can have additional benefits that extend beyond pain management. The specific medications prescribed will depend on the patient's condition, the severity of their symptoms, and their overall medical history. Medications can play a role in managing various aspects of VCDs, including addressing inflammation, reducing swelling, and preventing complications.
Some ways that medications help treat vascular compressions beyond just pain relief include:
•Reducing inflammation - Anti-inflammatory drugs such as NSAIDs and corticosteroids help decrease acute inflammation responsible for nerve and vessel irritation, edema and impaired mobility. By calming inflammation, these agents improve circulation and open passageways to relieve pressure and resolve symptoms. They are especially useful for neurogenic compressions and to reduce severity/frequency of acute flare-ups in conditions like median arcuate ligament syndrome or effort thrombosis.
•Relaxing muscle spasms - Muscle relaxants release spasms and high muscle tension contributing to thoracic outlet syndrome, celiac plexus compression and other entrapment disorders. By relaxing muscle tightness and spasticity, more space is created around compressed structures. These medications provide both short- and long-term benefits for muscle-related compressions when used intermittently or chronically as needed.
•Managing scar tissue - Antifibrotic drugs help minimize formation of dense scar tissue following injury or surgery for a compressive disorder. Excessive scarring may entrap nerves and vessels as thoroughly as the original problem. These medications aim to promote flexible, pliable scarring that does not significantly restrict movement or limit function as healing progresses. They are often used short-term post-operatively.
•Improving circulation - Vasodilators open arteries and veins to enhance blood flow which is restricted by stenosis or occlusion causing many vascular compressions. By improving both arterial perfusion and venous return, these medications relieve ischemia, reduce edema, and resolve circulatory symptoms such as pain, numbness, fatigue and skin changes. They may allow arterial and venous collateral branches to develop, stabilizing disease progression for certain conditions.
•Reducing excess fluids - Diuretics help lower fluid volume and decrease edema in cases where high venous pressure from obstruction or poor lymphatic drainage leads to substantial swelling and tissue changes. By sensitively reducing fluid levels, diuretics provide relief from pain and heaviness while improving mobility and tissue perfusion.
•Managing other conditions - Comorbidities such as diabetes, atherosclerosis or blood clotting disorders can influence both development and treatment of vascular compressions. Medications for these conditions aim to optimize circulation and health in general which in turn benefits compressive symptoms and outcomes. Tight glucose control, antiplatelets and medications to lower blood pressure/cholesterol may have significant impact.
•Supporting mood - Antidepressants and anticonvulsants in low doses help regulate mood and response to chronic pain which accompanies many longstanding compressions. By elevating pain tolerance and limiting distress, quality of life is improved. These medications enable a more positive outlook to cope with what may be lifelong management and adaptation to a persistent anatomical condition.
It is important for patients to understand the purpose and potential benefits of their prescribed medications and to work closely with their healthcare providers to ensure they are using these medications safely and effectively. Medications can be a valuable component of a comprehensive treatment plan for various VCDs when used in conjunction with other interventions such as physical therapy, lifestyle modifications, and, in some cases, surgical interventions.
Stay tuned for the next post in of this series, where we will explore another common misconceptions about VCDs...
About the Creator
Mohammad Barbati
Mohammad E. Barbati, MD, FEBVS, is a consultant vascular and endovascular surgeon at University Hospital RWTH Aachen. To date, he has authored several scientific publications and books regarding vascular and venous diseases.






Comments
There are no comments for this story
Be the first to respond and start the conversation.