The Arteries and Arterial System in the Human Body
An In-Depth Exploration

The human body is a miraculous network of interconnected systems, and the arterial system is one of the most vital. Arteries are the conduits that distribute oxygen-rich blood from the heart to every other part of the body.

Structure of Arteries
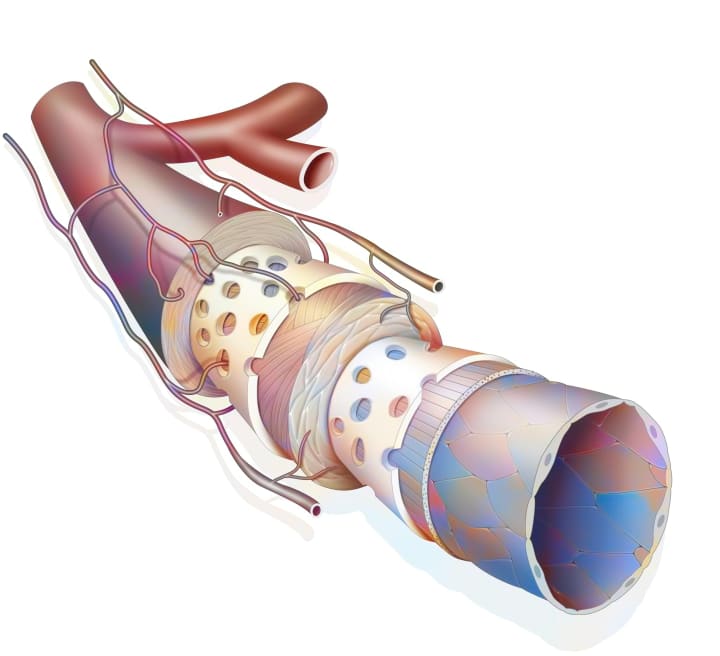
Arteries are composed of three layers: the intima, the media, and the adventitia.

Tunica Intima (Inner Layer): This is the innermost layer that is in direct contact with the blood flowing through the artery. It is composed of a thin layer of endothelial cells which are smooth and offer minimal resistance to blood flow. The tunica intima also includes a sub-endothelial layer made up of connective tissue containing elastic fibers.
Tunica Media (Middle Layer): The tunica media is the thickest layer and consists primarily of smooth muscle cells and elastic tissue. This layer plays a crucial role in controlling the diameter of the artery, thus regulating blood pressure and flow rate. It allows the artery to expand and contract with each heartbeat, a phenomenon known as vasodilation and vasoconstriction, respectively.
Tunica Adventitia (Outer Layer): The outermost layer is the tunica adventitia, comprised of connective tissue, collagen, and elastic fibers. It provides structural support and protection to the artery. This layer also contains tiny vessels known as vasa vasorum that supply blood to the outer wall of the artery.
Arteries can be further categorized into three types based on their size and function:
Elastic Arteries: These are the largest arteries (e.g., the aorta and its major branches) and have a large number of elastic fibers in the tunica media, allowing them to stretch and recoil with each heartbeat, smoothing out the pulse pressure generated by the heart's contractions.
Muscular Arteries: These arteries, also known as distributing arteries, have a thicker tunica media with more smooth muscle and fewer elastic fibers compared to elastic arteries. They are involved in vasoconstriction and vasodilation to regulate blood flow to different parts of the body.
Arterioles: These are the smallest arteries and they lead to the capillary beds. Arterioles have a relatively thick tunica media in relation to their lumen size. They play a crucial role in regulating blood pressure and flow into the capillaries.
Overall, the structure of arteries is specially designed to transport blood under high pressure, respond to changes in blood flow demand, and deliver oxygen and nutrients efficiently to all parts of the body.
Blood Pressure and the Arterial System
Blood pressure is an essential aspect of the cardiovascular system's function and health. It is the force exerted by circulating blood against the walls of the body's arteries, the primary vessels responsible for carrying oxygenated blood away from the heart.
As we age, our arterial walls can naturally become less elastic, leading to arteriosclerosis, or hardening of the arteries. It is generally found that pre-menopausal women are less likely to develop atherosclerosis than men of the same age due to the protective effects of estrogen. However, this protection wanes after menopause, equalizing the risk between genders.

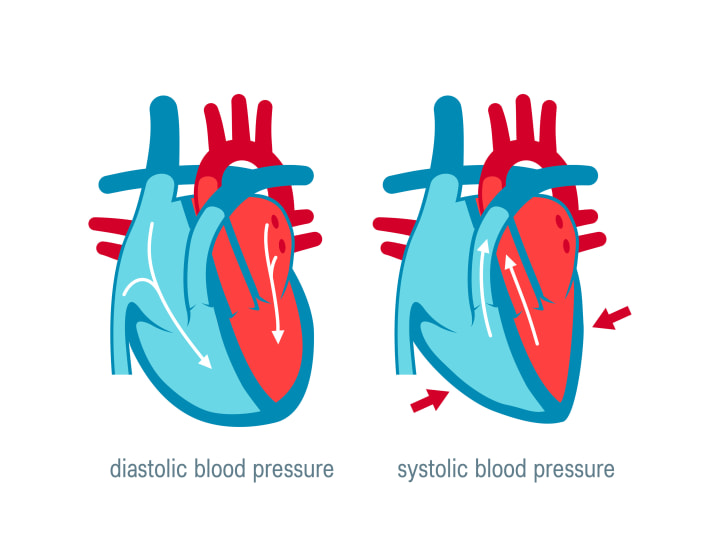
There are two components to blood pressure: systolic and diastolic pressure. Systolic pressure is the highest pressure, occurring during the contraction of the heart's left ventricle. Diastolic pressure is the lowest pressure, occurring when the heart's ventricles are filled with blood during relaxation.
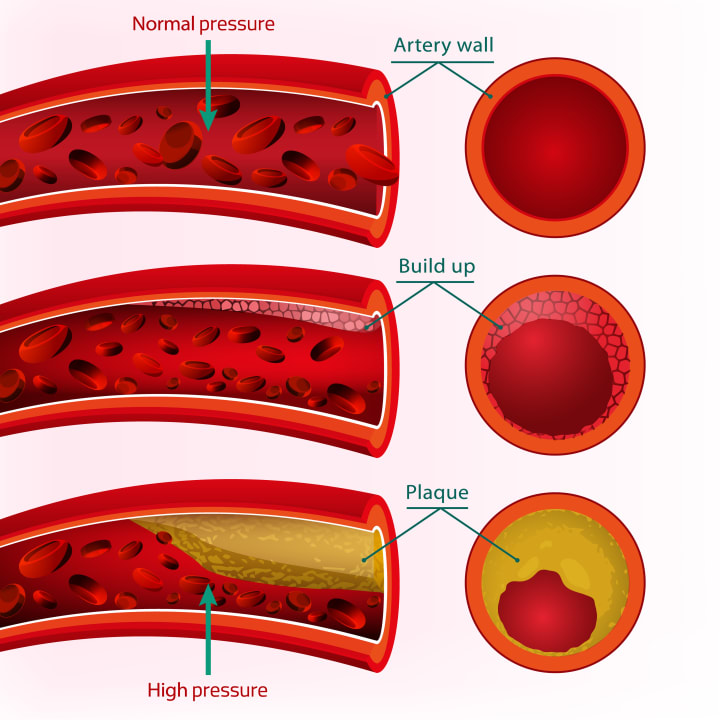
High blood pressure, or hypertension, is a condition where the force of the blood against the artery walls is consistently too high. Over time, this increased pressure can cause damage to the arterial wall, leading to a condition known as atherosclerosis. Atherosclerosis involves the buildup of fatty substances, cholesterol, cellular waste products, calcium, and fibrin (a clotting material in the blood) in the arteries.
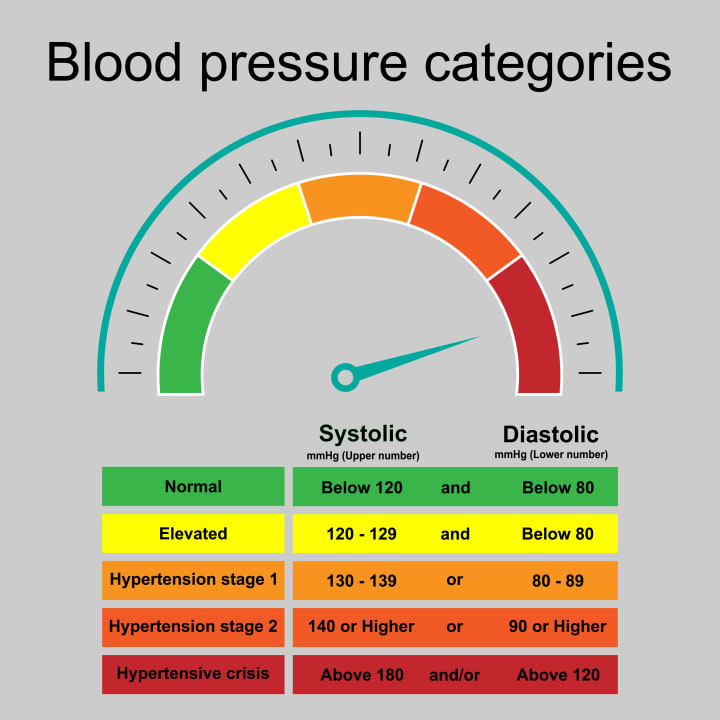
This buildup, known as plaque, hardens and narrows the arteries, limiting the flow of oxygen-rich blood to the body's organs and tissues. Depending on which arteries are affected, atherosclerosis can lead to a heart attack, stroke, or other serious vascular diseases.
Hypertension can also cause the arteries to stiffen over time, a condition known as arteriosclerosis. This loss of elasticity can further increase blood pressure, creating a vicious cycle of arterial damage.
On the other end of the spectrum, low blood pressure, or hypotension, can also pose challenges. Although it's generally considered less harmful than hypertension, severe hypotension can result in insufficient blood flow to the body's vital organs, potentially leading to stroke, heart attack, or kidney failure.
Maintaining a healthy blood pressure is crucial for arterial health. Regular exercise, a balanced diet, limiting salt and alcohol, avoiding tobacco, and managing stress can all contribute to maintaining a healthy blood pressure. Medications may also be necessary in some cases. Regular check-ups with a healthcare professional are essential for monitoring blood pressure and managing any health concerns promptly.
Changes with Age and Relation to Gender
Blood pressure is an essential aspect of the cardiovascular system's function and health. It is the force exerted by circulating blood against the walls of the body's arteries, the primary vessels responsible for carrying oxygenated blood away from the heart. As we age, the walls of our arteries naturally thicken and become less elastic, a process known as arteriosclerosis. This hardening of the arteries can lead to increased blood pressure, as the arteries are less able to expand and contract with each heartbeat.
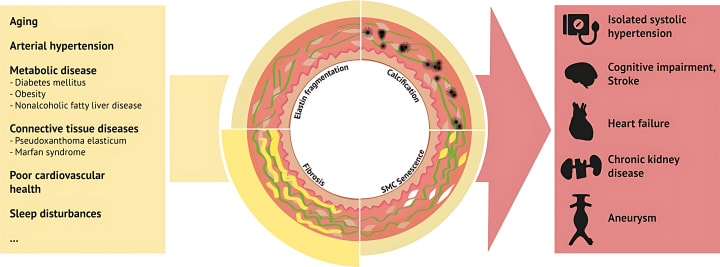
Arteriosclerosis is a significant risk factor for cardiovascular disease. As the arteries harden, it becomes more difficult for blood to flow freely through them, which can lead to the formation of blood clots. These blood clots can cause heart attacks or strokes if they block blood flow to the heart or brain, respectively.
Age also affects the body's ability to repair damage to the arterial walls. This decreased ability to heal, combined with an increased risk of damage due to conditions like hypertension and atherosclerosis, can lead to a higher incidence of arterial disease in older adults.
Gender also influences arterial health. Before menopause, women tend to have a lower risk of developing atherosclerosis and other arterial diseases compared to men. This is largely due to the protective effects of estrogen, a hormone that helps keep blood vessels flexible.
Estrogen helps to maintain the elasticity of arteries, reducing the risk of arteriosclerosis. It also has a beneficial effect on cholesterol levels, increasing 'good' HDL cholesterol and decreasing 'bad' LDL cholesterol, which can contribute to atherosclerosis.
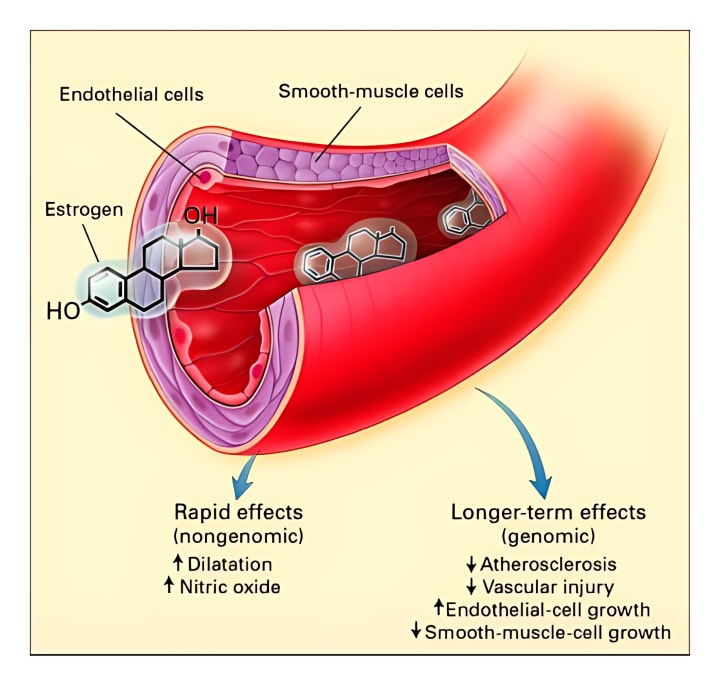
However, after menopause, women's risk of arterial disease increases. Estrogen levels drop significantly during menopause, which means that the protective effects of this hormone are reduced. As a result, post-menopausal women have a risk of developing arterial diseases that is similar to that of men.
Understanding these changes can help in the early detection and prevention of arterial diseases. Regular check-ups, a healthy lifestyle, and, in some cases, medication, can help manage these risk factors and maintain arterial health as we age.
Impact of Lifestyle: Smoking and Diet
The way we live our lives, including our dietary habits and whether we smoke, can significantly impact the health of our arterial system. These lifestyle choices can either protect or harm our arteries, influencing our risk of developing various arterial diseases.

Smoking is a major risk factor for arterial diseases. It can cause damage to the endothelium, the innermost lining of the arteries, which can lead to atherosclerosis.
When you smoke, you inhale a variety of harmful chemicals, including nicotine, carbon monoxide, and oxidizing chemicals. These substances can cause inflammation and damage to the arterial walls, promoting the buildup of plaque, a combination of fats, cholesterol, and other substances.

Smoking also reduces the level of high-density lipoprotein (HDL), or "good" cholesterol, in your body and increases the level of low-density lipoprotein (LDL), or "bad" cholesterol. This imbalance can contribute to plaque formation.

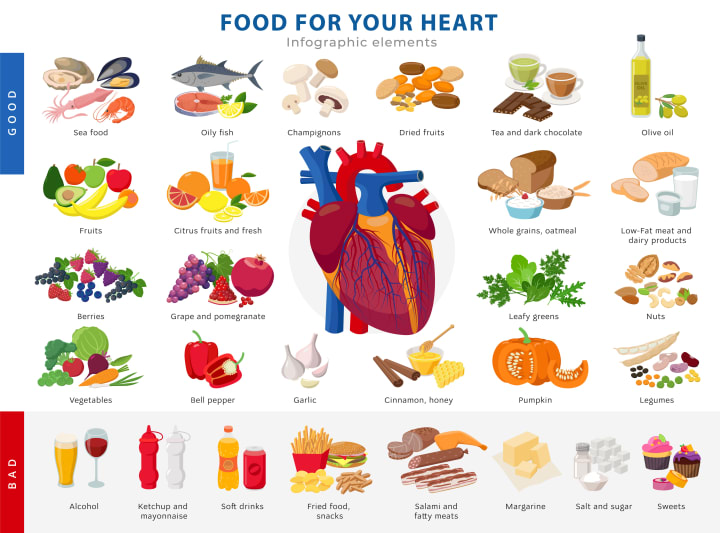
What we eat plays a significant role in the health of our arteries. A diet high in saturated and trans fats, cholesterol, and sodium can contribute to high blood pressure and the buildup of plaque in the arteries.
Saturated and trans fats increase the level of LDL cholesterol in the body, which can lead to atherosclerosis. High sodium intake can increase blood pressure, putting extra strain on the arteries and the heart.
On the other hand, a diet rich in fruits, vegetables, whole grains, lean proteins, and unsaturated fats can help protect arterial health. These foods provide essential nutrients and fiber, which can help control blood pressure and cholesterol levels.
The Role of Genetics in the Arterial System
Genetics can significantly influence the health of our arterial system. Certain genes we inherit from our parents can make us more susceptible to developing arterial diseases. Understanding this role can be instrumental in predicting, managing, and treating these conditions.
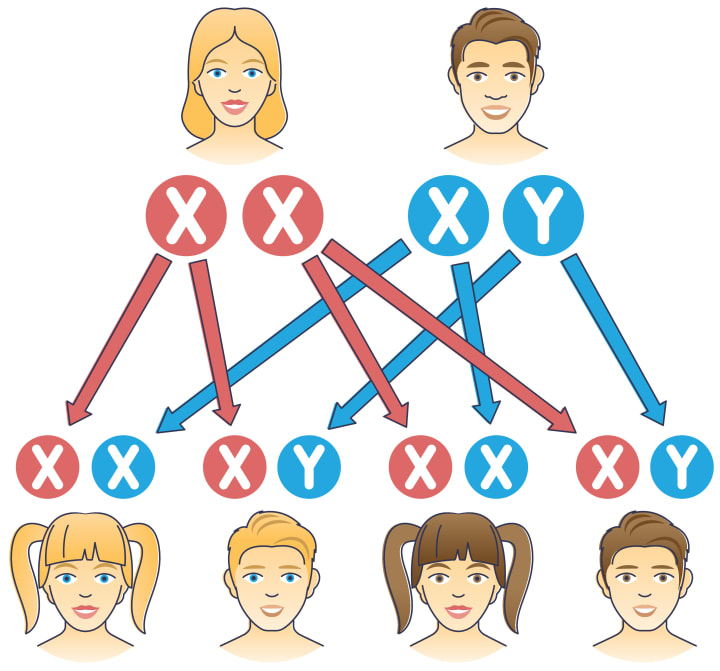
Genetic factors can predispose an individual to conditions like high blood pressure and high cholesterol, which can lead to arterial diseases like atherosclerosis. For instance, specific variants of the APOE gene affect the metabolism of fats in the body, influencing cholesterol levels and subsequently, the risk of atherosclerosis.
Additionally, certain genetic disorders can directly impact the health of the arterial system. For example, Marfan syndrome, caused by mutations in the FBN1 gene, can lead to the weakening of arterial walls and the development of aneurysms. Similarly, Ehlers-Danlos syndrome, caused by mutations in several genes, including COL5A1, COL5A2, and COL3A1, can result in fragile arteries that are more prone to dissection or rupture.

It's important to note that most arterial diseases are multifactorial, meaning they are caused by a combination of genetic, environmental, and lifestyle factors. For example, while genetics can predispose an individual to high cholesterol, dietary choices heavily influence cholesterol levels as well.
Balancing Factors and Challenges in Maintaining Arterial Health
Maintaining a healthy arterial system is a balancing act that requires careful consideration of various factors such as genetics, age, gender, and lifestyle choices. Each of these elements can significantly impact arterial health, and balancing them effectively can pose several challenges.

Understanding the arterial system is crucial for our overall health. By looking after our arteries, we can reduce the risk of serious conditions like heart disease and stroke, and live healthier, longer lives.
About the Creator
Mohammad Barbati
Mohammad E. Barbati, MD, FEBVS, is a consultant vascular and endovascular surgeon at University Hospital RWTH Aachen. To date, he has authored several scientific publications and books regarding vascular and venous diseases.






Comments
There are no comments for this story
Be the first to respond and start the conversation.