The pharmacy of the future
With an underfunded NHS and aging population there are enormous challenges ahead for UK healthcare. But springing up to meet them are new technologies offering greater accuracy and efficiency, better ways to engage with patients and more personalised care as well as making better use of scant resources. It’s a form of digital disruption that will open up new opportunities as the role of pharmacies changes in line with NHS and patient needs. So how will tomorrow’s pharmacies use new technologies to empower themselves, their business and their customers? We take a look at some of the options.
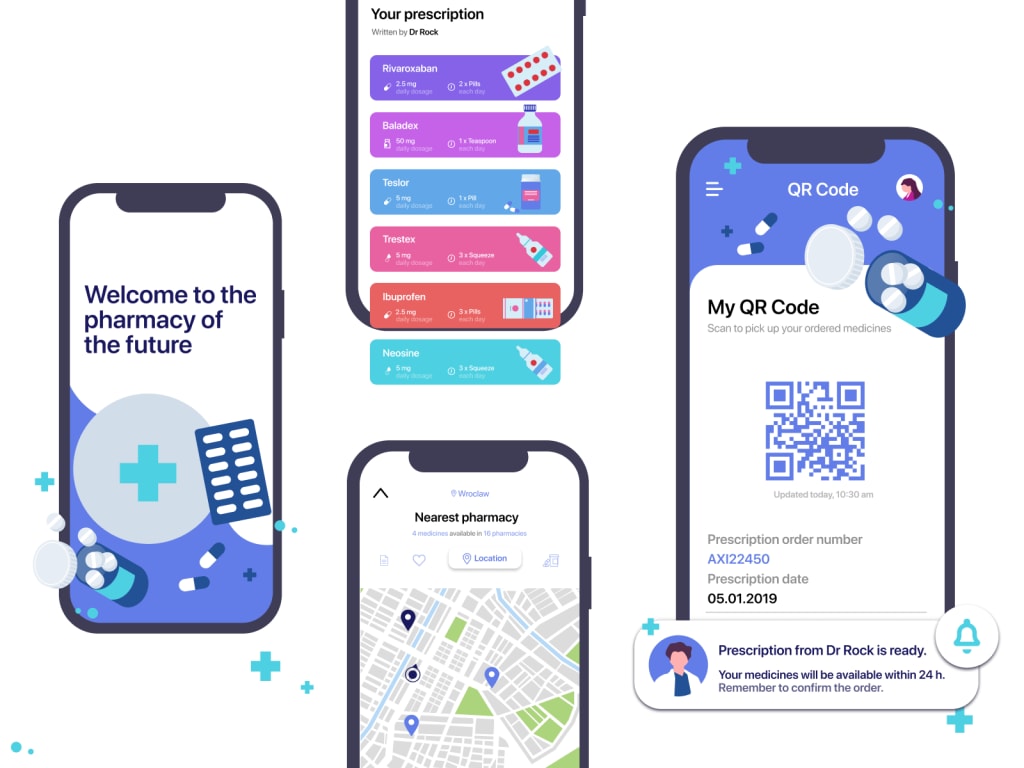
The NHS Long Term Plan for the future, published in January 2019, includes the role of community pharmacies and how they will fit in to the future NHS. In short, pharmacists will need to make better use of technology and team members’ skills; they will need to interact with patients digitally as well as updating their own skills to provide the services required by the NHS. Another report by the Royal Pharmaceutical Society ‘Now or never: shaping pharmacy for the future’ similarly stresses a shift of focus away from the simple supply of medicines towards the provision of services based around people’s needs. It brings together practical ideas about future models of care and talks about the challenges and opportunities for the pharmacy profession against a background of NHS reforms and new possibilities offered by technology. In another article for Pharmacy Magazine Professor Darrin Baines, an expert in economics and health technology, suggests that community pharmacies should be transformed into “technology hubs” to allow patients to connect with their pharmacy, local doctors, the wider healthcare system, pharmaceutical companies, charities, as well as other patients. So, what kind of innovations are we likely to see?
Robots to make up your prescription
One of the areas in which intelligent machines can help pharmacists and reduce the possibility of potentially dangerous errors is in dispensing. As recently as April 2019 a 65-year old Kent woman died after a pharmacist dispensed a wrongly-labelled blood pressure drug instead of pain relief medication. Automated dispensing technology eliminates human error and though the initial cost is significant at between £50,000-£500,000, in theory they will pay for themselves within 1-3 years. Although the technology has largely been adopted in UK hospitals, in local pharmacies we’re currently lagging behind. In Denmark almost 70% of community pharmacies have moved to dispensing robots and the figure is an estimated 30-40% of pharmacies in Europe. In the UK it’s less than 10% but those who are using them are keen advocates. Aberdeenshire pharmacist and tech enthusiast Galen Will is one of market-leading medical tech company BD Rowa’s 8,000 UK customers, saying “There are many benefits, such as accuracy, safety, dispensing efficiency and date rotation”. Thackers Pharmacy in Manchester is another example cited by the Royal Pharmaceutical Society, installing a dispensing robot that speeded up dispensing times, improved stock control and saved space that was turned into three patient consultation rooms. It also allowed the pharmacists to focus on clinical services and other areas. An unexpected bonus is the interest the technology creates with the public – there’s been more than one ‘name the robot’ competition in the last few years.
Michel Jürgens, sales director at BD says that automated dispensing ‘offers an opportunity to change how dispensing works’. So, what’s holding UK pharmacies back? As well as the initial investment, it may be down to worries about reliability, though evidence suggests the automated technology is reassuringly stable and accurate, with service agreements covering rare problems. There are also worries about job cuts, though the experience of Galen Will negates that – in fact he had to hire more staff to deal with the increase in turnover that resulted from adopting the technology. Perhaps it’s also because there’s no government decree, it’s up to individual pharmacies and pharmacy groups to take action and so far, only a small proportion have been brave enough to make the investment and actually do it.
New ways to engage with patients
With local GPs and the NHS under enormous pressure, future pharmacies reinvigorated by everyday technology like text messaging, live chat and video calling combined with better delivery services could play a larger role in patient care. Treating everyday illnesses through digital channels would take the strain off local GPs – not to mention lessen the chances of patients spreading non-serious but tiresome ailments to those who may be more vulnerable in the GP’s waiting room. In the U.S. some pharmacy chains already provide ‘live chat’ with a pharmacist on their websites, and the NHS is also launching an online service, concentrating on two areas: contraception and colds & flu. In Scotland it’s easier for pharmacists to manage patients with long-term conditions or minor ailments because local pharmacies and GP practices are already electronically linked; this is crucial in the rest of the UK to enable pharmacies to take on a bigger role.
The growing need for long-term treatment management
The digital revolution has resulted in people wanting more control over their care. Many of us can’t resist consulting Dr Google in the first instance, but information on the internet is overwhelming and can be contradictory. There’s an increasing need for treatment management; our aging population means there’s a growing number of people with long-term health problems who are on numerous different prescription medications, with 24% of adults report taking three or more prescribed medicines. GPs are advised to prescribe the cheapest version of a drug at that particular time, meaning patients can be prescribed a different brand with a different name from one month to the next, a system that unsurprisingly leads to confusion. Then there’s the difficulty of understanding how different medications interact with each other, or whether it’s possible an overworked GP who hasn’t read their full medical history has prescribed something unsuitable because of a pre-existing condition. Although some if not all of this information may be included in the patient information leaflet that comes with prescription medicine, the small print and indigestible format may lead to it being ignored. There is an opportunity here for pharma brands in conjunction with pharmacists and other healthcare providers to provide the reliable, objective information and tools that patients are looking for. But they need to remember that if there’s any sense that they’re simply pushing product, adoption will be low. Only by supporting outcomes rather than specifically focusing on the medications they sell will pharma companies overcome issues of trust and reach a wider audience.
Big pharma brands are already making some moves in this direction. AstraZeneca’s Day-by-Day mobile coaching app, delivered in partnership with Vida, is designed for patients who are recovering from a heart attack. The app is unbranded and can be used by any user, not just those taking the company’s drugs. In return the company will learn how patients are using their medications as they recover. In the future a digital assistant powered by machine learning that could offer personalised advice based on someone’s medical history, current health and treatment could potentially provide an additional, perhaps even better service than overstretched GPs. But perhaps a more pleasing alternative for pharmacists might be to adopt the approach set out by Eric Kinariwala, founder and CEO of New York City-based Capsule pharmacy. In an article for virgin.com he said ‘Rather than trying to develop technology to supplant [pharmacists], we built a technology platform designed to turn them into super-pharmacists – able to quickly use data to give consumers the right advice based on their behaviours and history. We used technology not to replace people, but as a way to make people better.”
Changing times, changing roles
The role of community pharmacies and pharmacists is growing and changing, and pharmacists everywhere should be emboldened by the successes in both patient treatment and business shown by digital pioneers. Bringing in new technologies should not be a way of simply cutting costs but instead allow pharmacists to focus on other services provided within pharmacies or via digital means. There are opportunities to learn new skills and take on a new role, not trying to replace GPs but as a trusted advisor in what will become an ever more important part of the healthcare ecosystem. In addition, if they can learn how to do it successfully there are opportunities for pharma brands to engage directly with customers in a way that has always proved challenging.
This is digital disruption brought to the pharmacy’s door but ultimately it will mean better patient pathways, closing the circle between patient, pharmacy and doctor. Perhaps a return to the more personalised service of yesteryear when people would have a proper relationship with a family doctor they’d seen for years, rather than being given a maximum 10-minute appointment with a stranger. Of course, whether that’s provided by a super-pharmacist assisted by digital technology or an AI who knows which hay fever medication you’re allergic to remains to be seen
Robotic surgery, 3D-printed prosthetics, and bionic organ transplants — modern medical technology can do the seemingly impossible in pursuit of saving lives. Yet as public attention is focused on innovation within health-care settings, the most profound advancements are those that affect patients well before (and often long after) they land in a doctor’s office or hospital room. These innovations aimed at improving the health experience are poised to transform the health-care industry from the inside out — and it’s easy to see why.
According to a recent Black Book survey, 92 percent of health-care consumers believe that improving the health experience should be a central focus when deploying digital health-care tools. This same survey found that 90 percent of patients feel no obligation to stay with a provider who does not offer a satisfactory digital experience.
The message is clear: modern health-care consumers expect exceptional care not only within hospitals and doctor’s offices but also beyond them. Health-care brands have no choice but to change the way they think about the health journey. From leveraging wearable technology to self-service digital pharmacies, here are some of the ways companies are bringing the health experience full circle — and shaping the future of the industry in the process.
Millennial health-care consumers are changing the way physicians and patients approach wellness. Studies exploring the shopping patterns of millennials suggest that this generation is more health conscious than any other generation before it, opting for health-focused diets and lifestyle choices — even when those choices cost them more money.
So it comes as no surprise that millennials are harnessing wearable tech to monitor, track, and analyze their health in real time — and brands are taking notice. The Apple Watch 4, released in September 2018, includes a built-in electrocardiogram that notifies wearers if it detects signs of an irregular heartbeat that would warrant a doctor’s visit. In response, insurer Aetna announced plans to subsidize the cost of Apple Watches for customers to support better health outcomes.
Consider how brands could significantly improve outcomes through wearable tech by creating more proactive wellness scenarios for patients. Imagine if data gathered from these wearable devices could help physicians by reminding patients of upcoming appointments, alerting them to possible health issues that even patients aren’t aware of, and even empower them to better diagnose and monitor patients with concrete data. Health-care brands that actively promote their customers’ overall well-being would ultimately boost loyalty and remain top-of-mind when their patients do fall ill
The self-reliance revolution has given rise to everything from online stylist services to AI-powered banking apps, but no industry has felt the impact of this trend more profoundly than health care. In the era of WebMD, health-care consumers are seeking answers via digital channels before heading to their doctor’s office (and sometimes in lieu of a visit altogether).
Brands have responded by offering their own healthcare portals that balance the benefits of a digital self-serve environment with expert advice. Insurance provider Oscar, for example, allows users to chat with physicians about their health questions and concerns without ever having to make an appointment. The app even integrates with a phone’s built-in pedometer to track steps and reward users for hitting certain milestones.
Health-care brands that utilize digital channels in this way are doing more than improving patient outcomes. Because customers will pay more for a fast, intuitive experience, innovative health-care brands such as Oscar are also boosting their bottom line
Even beyond the health-care setting, patients are turning to digital solutions to circumvent time-consuming visits to the pharmacy. Startups such as ScriptCenter MX and SpotRXare virtually eliminating the need for customers to ever directly interact with a pharmacist by replacing these interactions with digital kiosks and mobile apps.
These automated pharmacy machines (APMs) are popping up in office buildings, gyms, and even apartment complexes so that customers don’t need to venture beyond their daily commute to pick up prescriptions. Plus, research suggests that APMs promote patient safety by eliminating human error in drug refills. The accidental mix-up of drugs with similar sounding names, for example, is drastically reduced when patients use APMs.
Yet again, these innovations showcase how busy consumers prefer health care that comes to them, rather than the other way around. Creating faster and more convenient avenues for customers to do business with health-care brands will ultimately boost engagement
As consumers increasingly depend on digital channels to meet their health-care needs, brands that are too slow to make the shift will ultimately be left behind. Connected consumers may be more tapped into their health than ever before, but brands won’t be able to capitalize on this heightened awareness unless they invest heavily in upping their digital game.
Now more than ever, the health experience isn’t just about what happens once consumers walk into a hospital or doctor’s office. Brands that demonstrate a commitment to their customers’ health at every stage of their wellness journey will lead the way in the digital age
The future is digital reimagining patient engagement
Interactive patient systems provide a path forward, bringing much-needed efficiency to day-to-day operations for our caregivers, and providing patients and families with the comfort and information they need during one of the most difficult times in history
Long before the term Covid-19 was part of our vernacular, hospitals were experiencing rising rates of clinician burnout, and the complexity of our healthcare system was placing undue stress and anxiety on patients. But, the last year and a half has been unprecedented for our industry. Those in healthcare watch it unfold daily — the fear and exhaustion, the uncertainty spurred by required isolation levels and disjointed communications–the engagement gap will continue to widen if the industry does not act.
Though healthcare technology is not able to suit up and physically join the care team, and IT specialists might not be able to personally assuage patient fears, there are ways leaders in the healthcare IT space can help create environments that support care teams, patients, and families, to lessen or eliminate gaps in care and engagement.
It starts with setting the right tone for patients when they first enter the hospital room. Healthcare leaders must think of the hospital room as the patient’s space and leverage technology with the patient in mind. Modern patient engagement platforms can address a patient by name and personalize their care experience by delivering customized education, entertainment, and relaxation to their bedside. They can also transform formerly reactive devices such as the in-room TV into an interactive system that puts everything at the patient’s fingertips. As patients become more informed and start to feel like part of the care team, they can ask questions, raise concerns, and proactively prepare for discharge. It’s a simple way to provide patients with more meaningful interactions, while building deeper relationships, establishing trust, and ultimately fostering loyalty
Closing the engagement gap requires that technology supports the unique needs and specific workflows of the care team. Administrative tasks such as assigning and documenting educational content, updating dry-erase whiteboards, and triaging service requests, just to name a few, can consume a clinician’s workday. Patient engagement platforms can integrate with existing technology like Real-time Location Systems (RTLS) to prompt the in-room TV or digital whiteboard to automatically display the name, photo, and title for incoming members of the care team. Healthcare technology has the power to build better relationships between clinicians and patients by removing administrative waste and enabling clinicians to practice at the top of their license, giving patients a greater sense of comfort and ease.
It becomes particularly crucial at discharge when closing knowledge gaps and ensuring patients are informed when going home can help to avoid costly readmissions. To optimize patient outcomes and properly manage expectations, providers must integrate discharge planning across the care continuum. Successful discharge planning starts at admission and continues throughout the course of inpatient treatment. Equipped with a data-rich patient engagement platform, providers can harness patient data from a variety of sources to streamline the discharge process, ensure the accurate transfer of information, improve post-discharge outcomes and ultimately enhance the overall patient experience.
Let’s say the patient is in the hospital for a total knee replacement. Rather than having a nurse bring the patient a thick stack of paperwork with forms to sign and discharge education materials to read, the entire process can be automated and paperless. Clinicians can now “prescribe” easily digestible videos for patients to watch on their TV or bedside tablet. Patients can view the videos whenever they want and as many times as they want, enabling repetition that’s so important for comprehension and recall, and closing crucial learning gaps. When patients leave the hospital more educated than when they arrived, readmission rates can be reduced and the potential for positive outcomes increases.
Another vital way to close the engagement gap is for healthcare providers to have real-time access to patient feedback. Surveys initiated through patient room technology focus on many aspects of the care experience that are important to patients and their families, such as access to care, communication with providers, and helpfulness of support staff. The surveys allow patients to report objectively on their experience – without having to feel anxious about giving constructive criticism or offending those on duty
Yet, engagement gaps aren’t only about clinical knowledge. Other requests, such as housekeeping services or a request for a chaplain can impact patient satisfaction. Real-time surveys delivered to the bedside periodically, or triggered by an event, enable the hospital to better address the unique needs of their patients or perform service recovery in a timelier manner. Patient engagement platforms can even integrate with building management systems to give patients the ability to control their environment to their comfort (room temperature, lights, or shades). By automating service requests to the corresponding department, hospitals reduce the patient’s wait time, increase accuracy of the request, and allow the nurse to concentrate on clinical issues.
For today’s hospitals, addressing patient engagement is not simply a business priority, but rather a moral imperative. Our caregivers are stretched too thin, and our system is overwhelmed. Healthcare consumers are expecting us to push forward and innovate at a rapid pace. Interactive patient systems provide a path forward, bringing much-needed efficiency to day-to-day operations for our caregivers, and providing patients and families with the comfort and information they need during one of the most difficult times in history
The rapid development of medical technology affects every aspect of medicine and healthcare. Even the seemingly most remote and ivory-tower-like institution isn’t impervious to digital health disruption. We are, of course, talking about the pharmacy.
Although these institutions play a crucial role in the healing process, the impression about pharmacists and their drug store is often that they offer a type of commercial/business-like service. The doctor prescribes the appropriate medicine with the appropriate instructions, and the pharmacist provides it in exchange for money. In short, a clear business.
However, with the medical technological revolution, traditional, clear-cut roles become a thing of the past. Empowered patients have more agency over their health, while new technologies support the democratisation of care; shifting the hierarchical doctor-patient relationship to a partnership level. As patients of the 21st century evolve, so must pharmacies and pharmacists in the age of digital health. They have to redefine their place in medicine as well. A simple drug dispenser will not be enough in a shared and community-based economy
as patients are the most underused resources of healthcare, pharmacists are the most underused resources of medicine.
Despite modern society moulding their profession into medical shopkeeping, pharmacists have much more to offer. They undergo a rigorous educational path comparable to that of physicians but are in a better situation to devote more time to patients.
A recent JAMA study even showed that patients visit community pharmacies more often than their primary care physicians. Those community pharmacists thus represent valuable access to a healthcare professional with the added bonus of having more face-to-face time to take advantage of.
The evolution of pharmacies and pharmacists’ role in the digital health era can take several pathways. In this article, we visualise 3 scenarios for this evolution, but the actual one can be a composite of these scenarios sharing similar features while taking a shape of its own. However, the aim is to better depict the possibilities so as to be prepared for what’s next in the practical world of pharma.
Visualising the future of pharmacies
With pharmacists and drug stores adapting to the digital health era, several aspects of the pharmacy setting will have to change. From adopting new approaches to letting go of older ones, the pharmacy of the future will pack a different look and a different role. Leading authorities in the pharmaceutical industry already recognise this need for change and share the same point of view.
Back in 2013, the Royal Pharmaceutical Society already emphasised in its report about the future of pharmacy the need for pharmacies to refocus their strategy of just supplying medicines towards providing services that attend to patients’ needs. Published in January 2019, the “NHS Long Term Plan” for the future included the need for pharmacists to employ digital technology to improve their services and better interact with patients.
To sum up, the basic concept of the future pharmacist covers the ancient “mediwitch” combined with the 21st century tech-guru and scientific professional. A mediwitch, who has a special place in a given community, knows their “patients’” histories and provides basic care for their illnesses with appropriate medicine (or in the middle-ages: herbs or infusions). A tech-guru who knows how to decipher data from health trackers and wearables and is able to provide the necessary care based on the data, and of course a real scientific professional who knows the basics as well as the latest developments in pharma and medicine in general
Such a mediwitch-tech-guru would come in handy in rural, remote or smaller communities that have significantly less access to pharmacies. This phenomenon has an impact even on the readmission data of hospitals. In rural areas, where people cannot find open pharmacies as often as necessary, researchers found that the readmission data was higher than in urban areas. If the ultimate goal is the improvement of the quality of healing, this phenomenon has to be changed as well.
Thankfully, technology is at our disposal to help. So let’s see 3 potential, tech-aided scenarios that could have a big impact on pharmacies.
Scenario 1 A boost in medical booths with pharmaceutical offerings
A rise in the adoption of medical kiosks to provide pharmaceutical services is the least-likely scenario. These refer to booths located in malls or food courts where patients can enter to have a basic health check and talk to a healthcare professional via telecommunication. Despite some promising offerings, such ventures have already proven to be unsuccessful. One such telemedicine kiosk startup, HealthSpot, went bust in 2015; even after reportedly raising over $40 million and forming a joint venture with the Cleveland Clinic.
Reasons for its failure are manifold from the overhead associated with building and delivering kiosks to the need to pre-arrange appointments. It wasn’t really healthcare on-demand, and technology has evolved past what these physical kiosks could offer; even our smartphones can achieve more. Whether it’s to keep track of suspicious skin moles, detect Alzheimer’s or measure vital signs such as temperature or oxygen saturation, smartphones are the real Swiss Knife of digital health.
Nevertheless, other companies are still treading along the medical kiosk path with pharmaceutical offerings to expand access to care. In October 2019, the OnMed Station started to operate in Tampa, Florida. The health kiosk offers telemedicine visits, remote diagnosis and features an automated dispenser for common medications like antibiotics and antihistamines. In comparison to HealthSpot, this kiosk is fully HIPAA-compliant, does not require human staff and can dispense medicine. Another example is that of the FDA-approved Consult Station from France-based HD4. Their medical booth includes telemedicine consultation with portable diagnostic tools such as an EEG and a stethoscope; not unlike those, you could connect with your smartphone.
Such booths can be adopted on a smaller scale, but given past hurdles, they might not see the widespread success that they hope to achieve. Moreover, since patients themselves have access to the same technology from the phone in their pocket, pharmacies aren’t likely to invest in such kiosks that have the same features.
Scenario 2 Health consultancies
Wait in line; show your doctor’s prescription; take your medicines; pay the bill. These commercial aspects of pharmacies are all too common. And this perception is all too often at the expense of exchanging important medical information. Ever decided not to ask questions about a drug and leave right after settling the bill because the line was so long? What about not asking about vitamins and recommendations for mineral supplements you were checking before arriving at the counter? Maybe the pharmacists themselves did not have time to spare for you anyway.
However, with the help of digital health offerings, pharmacies can change from the simple drug distribution machines that we’re used to and into health consultancies. This is the more likely scenario in the short-term given that technology and organisational schedules already enable it. Pharmacists will have the opportunity to provide basic care to patients with simple problems and/or provide health management consultations. This way pharmacies rise to almost the same level as that of primary care practices
One of the most important factors for this development is the grass-root approach to healthcare. This involves healthcare professionals – including pharmacists – providing proactive patient care in the location that is most convenient for the patient. When the actual presence of pharmacists is not possible, such solutions as telemedicine fall into place.
For example, Intouch Health and its telehealth network patients in remote areas of the U.S. have access to high-quality emergency consultations for stroke, cardiovascular, and burn services in the exact time they need it. Moreover, with telehealth, medical professionals in such towns and rural areas also have access to speciality services and patients can be treated in their own communities.
This is part of the so-called point-of-care diagnostics, which allows patient diagnoses in the physician’s office, in an ambulance, at home, in the field, or in the hospital. The results of care are timely and allow rapid treatment to the patient. In fact, with digital health tools, a whole department’s worth of diagnostic tools can fit in a briefcase.
A digital stethoscope like the Eko Core lets users livestream recordings for telemedicine purposes. Portable ultrasound devices like the Philips Lumify and the Clarius deliver real-time high-resolution ultrasound images. The Viatom Checkme Pro packs multiple sensors in a single, handheld FDA-approved device to measure ECG, pulse, temperature, sleep quality and more.
From a practical point of view, we see the biggest potential in this scenario as pharmacies could easily invest in those solutions and offer such diagnostic services. Pharmacists can further help patients analyse the data generated and derive meaningful conclusions from it.
In addition, pharmacists are particularly fit for this purpose as they have the time to dedicate; a luxury that most doctor-patient meetings simply don’t have.
Scenario 3 Pharmacies as specialised point-of-care
This final scenario takes it one step further in imagining the future of pharmacies. It depicts pharmacies as specialised point-of-care centres where personalised therapies are made possible. Such centres will 3D-print multiple medications on a single pill, sequence one’s genome and combine such offerings to customise dosages based on one’s genomic data. Automated dispensers can further load the pills onto delivery drones for at-home deliveries. Such centres will serve as a gateway to access advanced healthcare technologies conveniently.
These possibilities aren’t the figment of our imagination but are existing and available today. In mainland Europe, 30-40% of pharmacies use automated dispensers. Medical drone deliveries are routinely performed in Rwanda. Earlier this year, FabRx released the first pharmaceutical 3D printer to manufacture personalised medicines. Their M3DIMAKER allows for the printing of medicines according to the user’s manufacturing needs, which in some cases means one month’s medication (28 pills) in around 8 minutes! Direct-to-consumer (DTC) genetic testing kits are getting more affordable and could soon cost only $100. Similar DTC kits are also gaining traction
DTC kits will be a big item, likely to speed up faster due to COVID, in the coming 2-3 years,” Timothy Aungst, an Associate Professor of Pharmacy Practice at MCPHS University, Worcester, told The Medical Futurist. “I would expect to see business partnerships strengthen here, and companies like TruePill or Amazon or CVS to push it, possibly Walmart.”
However, even if some advanced technologies might get integrated in pharmacies sooner, this scenario is still a longer-term one; even if the technologies are already available to make it possible. “Yes, pharmacists could do it, but again, legal issues or payments need to be addressed despite it making sense,” Timothy Aungst added. Indeed, regulatory constraints could hamper this adoption. Nevertheless, such constraints are part of the process of enabling a secured and trusted adoption for the best patient outcomes.
The future of pharmacies will be human
Despite all the tech-talk, a constant element that will be an integral part of the pharmacy of the future is the human element. While in the background automated robotic dispensers will solve logistics and drones will handle deliveries, it’s the human pharmacy staff who will be present at the forefront of the pharmacy.
With robots handling menial, routine tasks, pharmacists will have more time to dedicate to patients, help them interpret the data from their wearables and tackle challenges requiring creativity. There are several good examples out there to demonstrate how these can decrease costs and increase the quality and range of the service pharmacies provide today. While in this article we discussed the scenarios that pharmacies can take, we also analysed the technologies that will lead to these scenarios in our e-book released earlier this year. If you are curious about the technologies shaping the future of pharma, we encourage you to grab a copy below
About the Creator
William Solano
https://videofunds.buzz/4852475553184810/ sign up to get a 10 US Dollar newcomer bonus! I made more than 200 US Dollars by watching the video here, so you can try it.





Comments
There are no comments for this story
Be the first to respond and start the conversation.