What are platelets and what is their role in blood?
Definition:
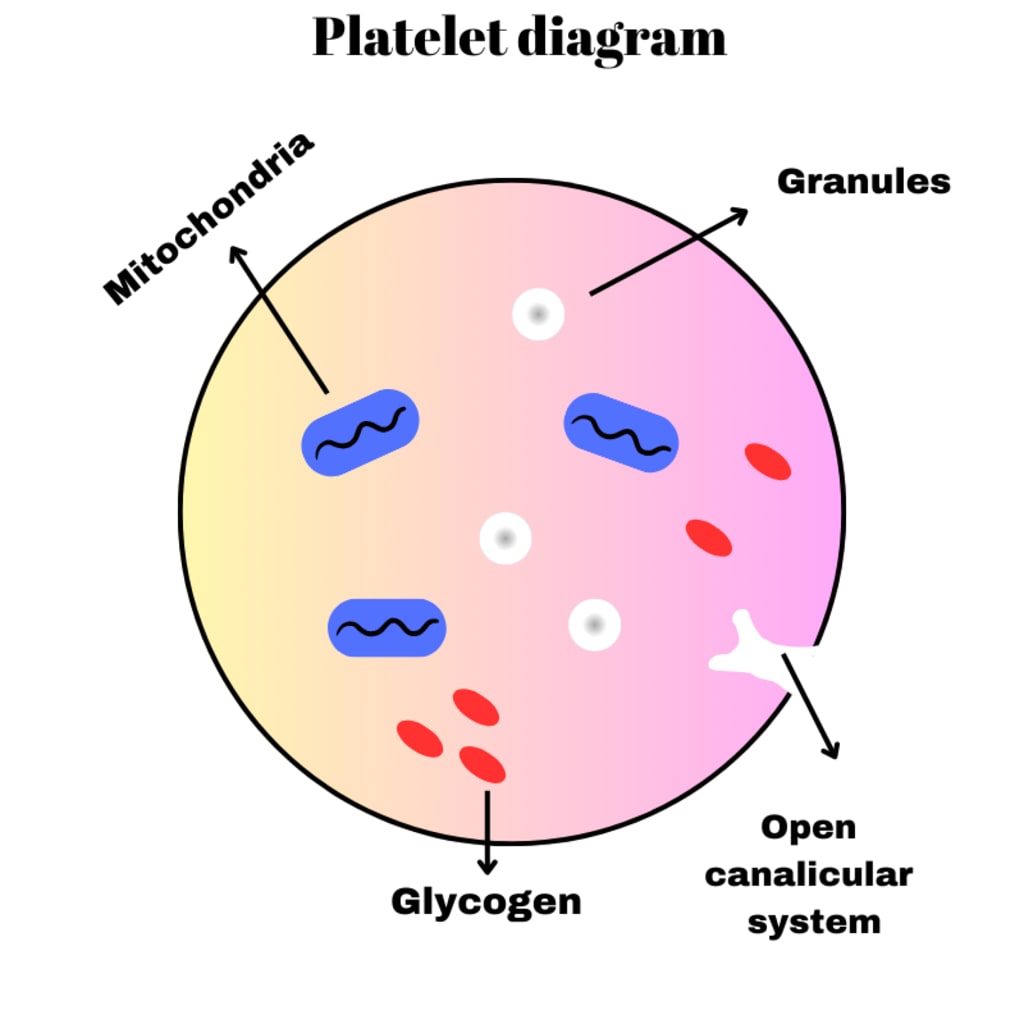
Platelets are otherwise called as thrombocytes. The word thrombocytes derived from Greek word “thrombos” meaning a “thick drop” or “clot”, and “cyte” means “cell”. These are very small non nucleated discs, produced from the cytoplasm of megakaryocytes in red bone marrow. Their size is about 2 to 4 µm diameter. Normal range of platelet count is between 2,00,000 to 3,50,000 per microliter or 200 x 109 /l and 350 x 109/l. Platelets contain variety of substances that promote blood clotting, which causes hemostasis.
Hemostasis:
When the blood vessel get ruptured or any injury can occurs, loss of blood is stopped by the series of overlapping processes, in which platelets play an important role. Hemostasis has done by following stages.
1. Vasoconstriction: When platelets come in contact with damaged blood vessels, their surface becomes sticky and they adhere to the damaged wall. They the platelets release serotonin (5-hydroxytryptamine), which constricts the blood vessel for reducing the blood flow through it. Thromboxanes are the other chemicals that cause the vasoconstriction.
2. Platelet plug formation: The adherent platelets clump to each other and release other substances, including adenosine diphosphate (ADP), which attract more platelets to the site. Passing platelets adhere to those already at the damaged vessel and they too release their chemicals. This is a positive feedback mechanism by which many platelets rapidly arrive at the site of vascular damage and quickly form a temporary seal. That is called platelet plug.
3. Coagulation: Coagulation is the blood clotting process that also involves a positive feedback mechanism and only a few stages are involved here. The factors involved are listed here.
Blood clotting factors:
Factor -I - Fibrinogen
Factor -II - Prothrombin
Factor -III - Tissue factor (thromboplastin)
Factor -IV - Calcium (Ca2+)
Factor -V - Labile factor, proaccelarin, Ac-globulin
Factor -VII - Stable factor, proconvertin
Factor -VIII - Antihaemophilic globulin (AHG), AH factor A
Factor -IX - Christmas factor, plasma thromboplastin
component (PTA), AH factor B.
Factor -X - Stuart Prower Factor
Factor -XI - Plasma thromboplastin antecedent (PTA), antihaemophilic factor C.
Factor -XII - Hageman factor
Factor -XIII - Fibrin stabilizing factor
Note: There is no factor VI.
Blood clotting results in formation of an insoluble thread like mesh of fibrin which traps blood cells and is much stronger than the rapidly formed platelet plug. In the final stages of this process Prothrombin activator acts on the plasma protein Prothrombin converting in to thrombin. Thrombin then acts on another plasma protein fibrinogen converts it to fibrin. After a time the clot shrinks, squeezing out serum, a clear sticky fluid that consists of plasma from which clotting factors have been removed.
4. Fibrinolysis: After the clot has formed the process of removing it and healing the damaged blood vessel begins. The breakdown of the clot, or Fibrinolysis, is the first stage. An inactive substance called plasminogen is present in the clot and is converted to the enzyme plasmin by activators released from the damaged endothelial cells. Plasmin initiates the breakdown of fibrin to soluble products that are treated as waste material and removed by phagocytosis. As the clot is removed, the healing process restores the integrity of the blood vessel wall.
Functions of platelets:
Hemostasis and Blood Clotting:
Adhesion: When a blood vessel is injured, platelets adhere to the exposed collagen fibers of the damaged vessel wall. This initial adhesion is essential for the subsequent steps in hemostasis.
Release Reaction: Once adhered, platelets release various substances stored in their granules, such as serotonin and ADP (adenosine diphosphate). These substances further activate nearby platelets, promoting the formation of a plug at the site of injury.
Aggregation: Activated platelets stick together (aggregate) through the binding of fibrinogen, forming a temporary plug or clot that helps seal the breach in the blood vessel.
Vasoconstriction:
Platelets contribute to the constriction of blood vessels (vasoconstriction) at the site of injury. This immediate response helps minimize blood loss by reducing the flow of blood through the damaged vessel.
Immune Response:
Platelets contain proteins and molecules that participate in the immune response. They can interact with immune cells and release factors that contribute to the inflammatory process, which is crucial for initiating the healing process after injury or infection.
Wound Healing and Tissue Repair:
Platelets release growth factors that stimulate cell proliferation and tissue repair. These growth factors play a significant role in the regeneration of blood vessels and connective tissue at the site of injury.
Antimicrobial Defense:
Platelets possess antimicrobial properties and can recognize and interact with pathogens, contributing to the immune response against infections.
Disease condition associated with platelets:
Thrombocytopenia:
Definition: Thrombocytopenia is a condition characterized by a low platelet count in the blood, typically below 150,000 platelets per microliter.
Causes:
Diminished creation of platelets in the bone marrow. Expanded annihilation of platelets in the circulatory system or spleen. Petechiae (little red or purple spots on the skin).
Symptoms:
• Easy bruising.
• Petechiae (little red or purple spots on the skin).
• Prolonged bleeding from minor injuries.
• Excessive bleeding during menstruation.
Conditions Associated:
• Immune thrombocytopenic purpura (ITP).
• Drug-induced thrombocytopenia.
• Thrombotic thrombocytopenic purpura (TTP).
• Hemolytic-uremic syndrome (HUS).
Thrombocytosis:
Definition: Thrombocytosis is a condition characterized by an abnormally high platelet count in the blood, usually exceeding 450,000 platelets per microliter.
Causes:
Reactive or secondary thrombocytosis can result from conditions like inflammation, infection, or surgery. Primary or essential thrombocytosis may be associated with myeloproliferative disorders, such as essential thrombocythemia.
Symptoms:
• Headache and dizziness.
• Weakness and fatigue.
• Thrombosis (formation of blood clots).
Complications:
Increased risk of clotting events, such as deep vein thrombosis (DVT) or pulmonary embolism.
Hemorrhagic Disorders:
Von Willebrand Disease (VWD):
A hereditary bleeding disorder caused by a deficiency or dysfunction of von Willebrand factor, a protein that helps platelets adhere to blood vessel walls.
Glanzmann Thrombasthenia:
An inherited platelet function disorder characterized by a deficiency or dysfunction of glycoprotein IIb/IIIa, a crucial receptor for platelet aggregation.
Platelet Function Disorders:
Bernard-Soulier Syndrome:
A rare inherited disorder characterized by a deficiency or dysfunction of glycoprotein Ib/IX/V, leading to impaired platelet adhesion.
Gray Platelet Syndrome:
A rare inherited disorder characterized by a lack of alpha granules in platelets, resulting in abnormal platelet function.
Disseminated Intravascular Coagulation (DIC):
Definition: A complex disorder characterized by widespread activation of coagulation, leading to both excessive clotting and bleeding.
Causes:
• Sepsis.
• Trauma.
• Cancer.
Symptoms:
• Bleeding from multiple sites.
• Organ failure.
• Microvascular thrombosis.
For more related articles, follow pharmacyinfos.com





Comments
There are no comments for this story
Be the first to respond and start the conversation.