Unraveling the Mysteries of Ehlers-Danlos Syndrome
A Closer Look at the Invisible Illness
What is it about?
Ehlers-Danlos Syndrome (EDS) is a group of inherited connective tissue disorders that affect an estimated 1 in 5,000 individuals worldwide. Despite its prevalence, EDS is often referred to as an "invisible illness" due to the wide range of symptoms and lack of awareness surrounding the condition. In this post, we will delve into the intricacies of EDS, its various subtypes, and the ongoing research that aims to improve the lives of those affected by this complex disorder.
Understanding Ehlers-Danlos Syndrome
At its core, EDS is a result of genetic mutations that affect the body's production of collagen—a vital protein responsible for providing structure and strength to our skin, bones, muscles, and connective tissues. With compromised collagen, individuals with EDS often experience joint hypermobility, skin that is easily bruised and hyper-elastic, and tissue fragility. There are currently 13 recognized subtypes of EDS, each with its unique set of symptoms and genetic origins.
The Many Faces of EDS
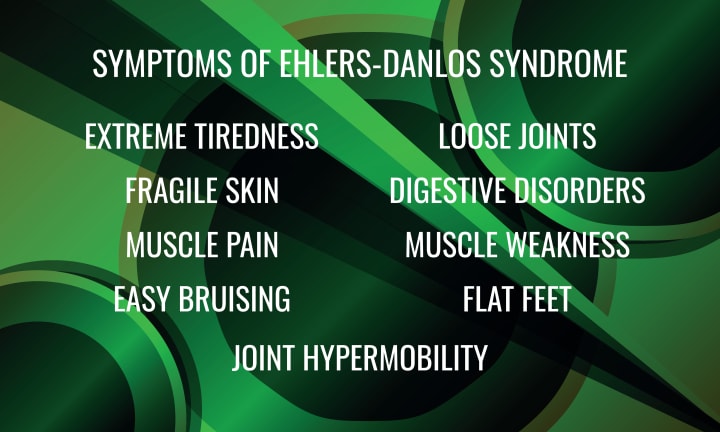
EDS symptoms can vary greatly from one individual to another, even within the same subtype. Some common symptoms include:
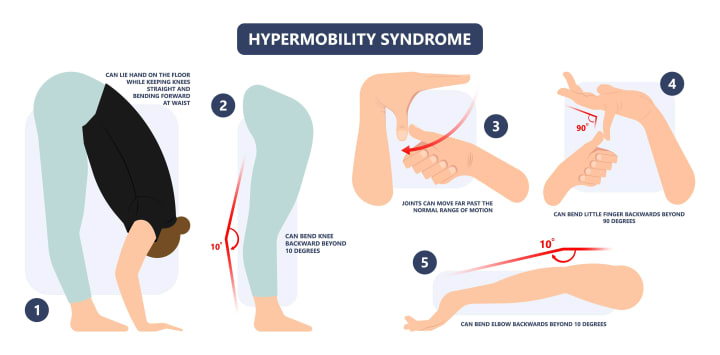
1. Joint hypermobility: Joint hypermobility refers to an increased range of motion in the joints, beyond what is considered normal. In EDS, this hypermobility can occur due to various factors, such as:
- Collagen structure and function: The genetic mutations in EDS can result in irregular collagen production, leading to weakened connective tissue surrounding the joints. This can cause joint laxity and make the joints more prone to dislocation and subluxation (partial dislocation).
- Joint capsule and ligament laxity: The joint capsule and ligaments surrounding the joint are composed of connective tissue. In individuals with EDS, the mutated collagen can lead to weakened and lax joint capsules and ligaments, allowing for greater joint mobility.
- Muscle imbalance and weakness: Due to the increased joint mobility, the muscles surrounding the joint may be required to work harder to provide stability. This can lead to muscle imbalances and weakness, further contributing to joint instability.
2. Skin elasticity and fragility: Skin hyperextensibility refers to the ability of the skin to stretch beyond the normal range and then return to its original position. In individuals with EDS, increased skin elasticity can occur due to:
- Altered collagen structure and function: The genetic mutations associated with EDS can lead to abnormalities in the collagen molecules themselves or in the enzymes responsible for processing and assembling collagen fibrils. This can result in a reduced amount of collagen or structurally abnormal collagen, causing the skin to be more elastic.
- Weakened connective tissue matrix: The weakened and disorganized collagen network in the skin can lead to a less structured and more elastic connective tissue matrix. This allows the skin to stretch more easily than in individuals without EDS.
Skin fragility refers to the propensity of the skin to bruise, tear, or scar easily. In individuals with EDS, skin fragility can be caused by:
- Impaired collagen structure and function: As mentioned earlier, the genetic mutations in EDS can lead to abnormalities in collagen production, assembly, or processing. This can result in a weakened and disorganized connective tissue matrix in the skin, making it more susceptible to injury.
- Reduced skin strength and integrity: The impaired collagen network can lead to reduced skin strength and integrity, making it more prone to bruising, tearing, or developing atrophic scars (thin, depressed scars).

3. Chronic pain: Chronic pain is a common and significant feature of EDS, affecting the majority of individuals with the condition. The pain in EDS can be multifactorial and complex, with several contributing factors.
- Joint instability and dislocations: The joint hypermobility in EDS can lead to joint instability, dislocations, and subluxations (partial dislocations), which can cause acute and chronic pain.
- Muscle and soft tissue pain: The increased joint mobility can place additional strain on the muscles, tendons, and ligaments surrounding the joints, leading to muscle imbalances, overuse injuries, and chronic soft tissue pain.
- Nerve pain and compression: In some cases, the joint instability and soft tissue laxity can lead to nerve compression or irritation, resulting in neuropathic pain.
- Chronic fatigue and pain sensitization: Chronic pain and fatigue can lead to central sensitization, a phenomenon in which the nervous system becomes more sensitive to pain signals. This can result in increased pain perception and reduced pain tolerance.
- Comorbid pain conditions: Individuals with EDS may be more prone to developing other chronic pain conditions, such as fibromyalgia, temporomandibular joint dysfunction, or chronic headaches.
4. Fatigue: Persistent exhaustion that may be exacerbated by poor sleep quality and chronic pain.
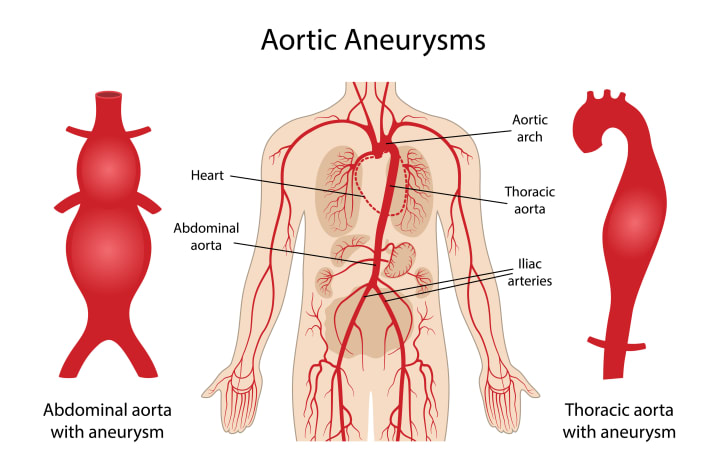
5. Cardiovascular issues: While EDS primarily affects the musculoskeletal and integumentary systems, it can also impact the cardiovascular system, leading to various issues and complications. The severity and prevalence of cardiovascular issues can vary depending on the specific type of EDS:
- Vascular Type (vEDS): The Vascular Type of EDS (vEDS) is the most severe form in terms of cardiovascular complications. Individuals with vEDS have a higher risk of arterial, intestinal, and uterine rupture due to the fragility of blood vessels and other hollow organs. This can lead to life-threatening internal bleeding and requires immediate medical intervention.
- Aortic root dilation: Some individuals with EDS, particularly those with the Classical Type (cEDS) or the Hypermobile Type (hEDS), may experience aortic root dilation. This refers to the enlargement of the aortic root, the section where the aorta connects to the heart. Aortic root dilation can increase the risk of aortic dissection or rupture, although the risk is generally lower in cEDS and hEDS than in vEDS.
- Mitral valve prolapse (MVP): MVP is a condition in which the mitral valve in the heart does not close properly, allowing some blood to flow backward from the left ventricle to the left atrium. This can cause symptoms such as palpitations, chest pain, or shortness of breath, although many individuals with MVP do not experience any symptoms. MVP is more common in individuals with EDS, particularly those with the Hypermobile Type (hEDS).
- Orthostatic intolerance and postural orthostatic tachycardia syndrome (POTS): Orthostatic intolerance refers to the development of symptoms, such as dizziness, lightheadedness, or fainting, upon standing or changing position. POTS is a specific form of orthostatic intolerance characterized by an excessive increase in heart rate when standing. Both orthostatic intolerance and POTS are more common in individuals with EDS, particularly the Hypermobile Type (hEDS), and can be associated with fatigue, exercise intolerance, and reduced quality of life.
Clinical Implications and Management
Joint hypermobility in EDS can have various clinical implications, such as:
- Pain and discomfort: The increased joint mobility can lead to chronic joint pain, discomfort, and fatigue, which can affect the quality of life for individuals with EDS.
- Joint instability and dislocations: The laxity in the joint capsule and ligaments can make the joint prone to dislocations and subluxations, which can be painful and potentially cause damage to the joint structures.
- Increased risk for osteoarthritis: The increased joint mobility and instability can lead to increased wear and tear on the joint surfaces, increasing the risk for the development of early-onset osteoarthritis.
- Impaired proprioception: The altered joint structure and function can affect an individual's ability to sense the position and movement of their joints, which can lead to difficulties with balance and coordination.
Management of joint hypermobility in EDS typically includes a combination of the following approaches:
- Physical therapy: A tailored physical therapy program can help to improve muscle strength and stability around the joints, reducing pain and the risk of joint dislocations.
- Joint protection strategies: Individuals with EDS may be advised to avoid activities that place excessive stress on the joints, such as high-impact sports or heavy lifting, to reduce the risk of injury.
- Orthotic devices: Braces or splints may be used to provide additional support and stability to the joints, particularly during activities that may place strain on the joints.
- Pain management: A combination of pharmacological and non-pharmacological interventions, such as medication, heat or cold therapy, and relaxation techniques, may be used to manage pain associated with joint hypermobility.
- Education and self-management: Understanding the condition and learning how to manage symptoms through appropriate activities, pacing, and lifestyle modifications is essential for individuals with EDS and joint hypermobility.
Increased skin elasticity and fragility in EDS can have various clinical implications, such as:
- Injury and wound healing: The fragile skin can be more susceptible to injury, leading to frequent bruising, tearing, and scarring. The altered collagen structure may also impair the wound healing process, resulting in slow or abnormal healing.
- Aesthetic concerns: The atrophic scars, visible veins, or other skin manifestations of EDS may cause aesthetic concerns for some individuals, impacting their self-esteem and overall quality of life.
- Vascular complications: In the Vascular Type of EDS, the increased skin fragility can be accompanied by a higher risk of arterial or organ rupture, which can be life-threatening. Thus, individuals with vEDS need to be closely monitored and managed for potential complications.
Management of skin elasticity and fragility in EDS typically includes a combination of the following approaches:
- Skin protection: Individuals with EDS should be advised to take precautions to reduce the risk of skin injury, such as wearing protective clothing, avoiding excessive sun exposure, and using gentle skin care products.
- Wound care: Proper wound care is essential to promote optimal healing and reduce the risk of infection. This may include keeping the wound clean, using appropriate dressings, and seeking medical advice for slow-healing or infected wounds.
- Topical treatments: Topical treatments, such as emollients or barrier creams, can help to maintain skin hydration and integrity, reducing the risk of skin injury.
- Lifestyle modifications: Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and adequate hydration, can help to promote overall skin health and resilience.
- Monitoring and management of vascular complications: For individuals with vEDS, regular monitoring for potential vascular complications and timely management, including surgical intervention if necessary, are crucial to reduce the risk of life-threatening complications.
The management of chronic pain in EDS is often challenging and requires a multidisciplinary approach. Some strategies for pain management include:
- Physical therapy and exercise: A tailored physical therapy program can help to improve muscle strength, joint stability, and overall function, which may help to reduce pain. Low-impact exercises, such as swimming or cycling, may be recommended to minimize stress on the joints.
- Pain-relief medications: Over-the-counter pain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen, may be used to manage mild to moderate pain. In cases of severe or persistent pain, stronger prescription medications, such as opioids, may be considered. However, their use should be carefully monitored due to the risk of dependence and side effects.
- Neuropathic pain medications: If neuropathic pain is present, medications specifically designed for nerve pain, such as gabapentin or pregabalin, may be prescribed.
- Alternative and complementary therapies: Some individuals with EDS may find relief from pain through alternative therapies, such as acupuncture, massage therapy, or chiropractic care. However, it is essential to work with knowledgeable and experienced practitioners who understand the specific needs and precautions associated with EDS.
- Cognitive-behavioral therapy (CBT): CBT can help individuals with chronic pain develop effective coping strategies, improve pain management, and reduce the impact of pain on their quality of life.
- Lifestyle modifications and self-management: Adopting a healthy lifestyle, including a balanced diet, regular exercise, stress management, and proper sleep hygiene, can help to improve overall health and well-being, which may have a positive impact on pain levels. Additionally, learning self-management techniques, such as pacing activities and using assistive devices, can help to reduce the strain on the joints and minimize pain.
- Multidisciplinary pain management: In some cases, individuals with EDS may benefit from a comprehensive pain management program that includes a combination of medical, physical, psychological, and alternative therapies.
The management of cardiovascular issues in EDS depends on the specific condition and the severity of the symptoms. Some general management strategies include:
- Regular monitoring: Individuals with EDS should undergo regular cardiovascular evaluations to monitor for potential complications, such as aortic root dilation or MVP. This may include physical examinations, echocardiograms, or other imaging studies.
- Lifestyle modifications: Adopting a heart-healthy lifestyle, including a balanced diet, regular exercise, stress management, and avoiding smoking, can help to promote overall cardiovascular health in individuals with EDS.
- Medications: In some cases, medications may be prescribed to manage cardiovascular issues in EDS. For example, beta-blockers or angiotensin receptor blockers (ARBs) may be used to manage aortic root dilation, while medications targeting the autonomic nervous system may be prescribed for POTS.
- Surgical intervention: In severe cases of aortic root dilation or arterial rupture, surgical intervention may be necessary to repair or replace the affected blood vessels or heart valves. For individuals with vEDS, surgery carries additional risks due to the fragility of the blood vessels and tissues, and careful preoperative planning is essential.
- Management of orthostatic intolerance and POTS: For individuals with orthostatic intolerance or POTS, conservative management strategies, such as increasing fluid and salt intake, wearing compression stockings, and practicing physical countermeasures (e.g., leg crossing, muscle tensing), may be recommended to alleviate symptoms. In some cases, medications may also be prescribed to manage POTS.
The Future of EDS Research
While researchers continue to unravel the complexities of EDS, recent advances in genetics have provided valuable insights into the disorder. By identifying specific gene mutations and understanding their impact on collagen production, scientists are laying the groundwork for potential targeted treatments and interventions.
One area of ongoing research is the investigation of modifier genes and their role in EDS. These genes may help explain the variability in symptom severity among individuals with the same genetic mutation. Additionally, researchers are exploring the potential impact of environmental factors on EDS symptoms and progression.
Final words
Ehlers-Danlos Syndrome remains a complex and poorly understood disorder, but with increased awareness and ongoing research, the future looks promising for those living with EDS. By deepening our understanding of the genetic underpinnings of the condition and identifying potential treatment targets, we can move closer to developing effective therapies and improving the quality of life for individuals with this invisible illness.
About the Creator
Mohammad Barbati
Mohammad E. Barbati, MD, FEBVS, is a consultant vascular and endovascular surgeon at University Hospital RWTH Aachen. To date, he has authored several scientific publications and books regarding vascular and venous diseases.






Comments
There are no comments for this story
Be the first to respond and start the conversation.