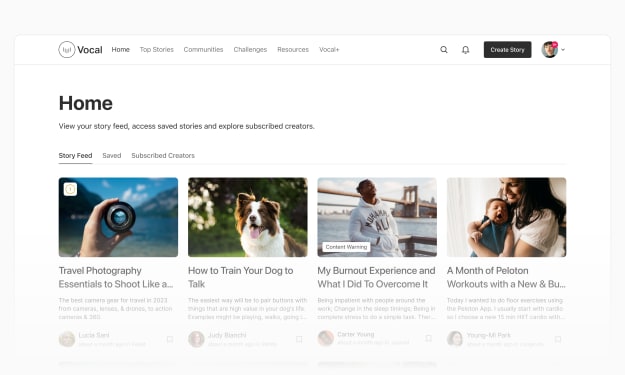
Content warning
This story may contain sensitive material or discuss topics that some readers may find distressing. Reader discretion is advised. The views and opinions expressed in this story are those of the author and do not necessarily reflect the official policy or position of Vocal.
TUBULOINTERSTITIAL NEPHRITIS
CAUSES, SYMPTOMS AND TREATMENT OPTIONS

Tubulointerstitial nephritis is a kidney disorder characterised by inflammation and damage to the tubules and interstitial tissue in the kidney. Various factors, including infections, medications, autoimmune diseases, and metabolic conditions can cause it. Symptoms may include decreased kidney function, blood in the urine, and electrolyte imbalances. Treatment aims to address the underlying cause and manage kidney inflammation.
Causes of Tubulointerstitial Nephritis
An allergic response to a drug is the most frequent cause of acute tubulointerstitial nephritis. Diuretics, nonsteroidal anti-inflammatory medications (NSAIDs), including aspirin, and antibiotics such as penicillin and sulfonamides can cause an allergic response. There is often a time delay of three to five weeks between the development of acute tubulointerstitial nephritis and the exposure to the allergen that triggered the reaction. Nonallergic processes can also result in tubulointerstitial nephritis caused by medications. For instance, chronic tubulointerstitial nephritis can be caused by NSAIDs directly, and it can take up to 18 months for this to happen.
Tubulointerstitial nephritis, acute or chronic, can also result from kidney infection (pyelonephritis). Unless pyelonephritis affects both kidneys or inflammation results in an obstruction in the urinary system, kidney failure is rare.
Immunologic conditions that primarily impact the kidney, such as interstitial nephritis linked with anti-tubular basement membrane (anti-TBM) antibodies, may cause tubulointerstitial nephritis.
Symptoms of Tubulointerstitial Nephritis
Some individuals experience little or nonexistent symptoms. The onset of symptoms is quite unpredictable and might come on abruptly or gradually.
Acute Tubulointerstitial Nephritis – Urine production may be normal or lower than usual in cases of abrupt tubulointerstitial nephritis. In some instances, people generate excessive amounts of urine, which causes them to pee more often and wake up throughout the night to urinate (nocturia). The symptoms of pyelonephritis include fever, uncomfortable urination, and lower back or side (flank) pain. Fever and rash may be present if the cause is an allergic response.
Chronic Tubulointerstitial Nephritis – Symptoms of kidney failure, including itching, weariness, decreased appetite, nausea, vomiting, and trouble breathing, initially manifest when tubulointerstitial nephritis develops gradually and gets worse. Early on in the course of the illness, blood pressure is normal or hardly elevated. There might be more pee generated than usual.
Treatment Options for Tubulointerstitial Nephritis
Treatment for tubulointerstitial nephritis primarily focuses on addressing the underlying cause and managing inflammation and kidney damage. Common treatment approaches may include
Discontinuing Offending Medications – If medications are the cause, discontinuing or changing them may be necessary.
Treating Infections – If infections are responsible, appropriate antibiotics or antiviral medications are prescribed.
Corticosteroids – In cases of autoimmune-related nephritis, corticosteroid medications may help reduce inflammation.
Supportive Care – Managing symptoms such as electrolyte imbalances, high blood pressure, and fluid retention.
Dialysis – In severe cases with significant kidney damage, dialysis may be required to help filter waste and excess fluids from the blood.
It’s crucial to consult a healthcare provider for an accurate diagnosis and appropriate treatment plan tailored to the specific cause and severity of tubulointerstitial nephritis.
If the underlying illness is effectively treated or the offending medicine is withdrawn, kidney function typically recovers. However, renal scarring is frequent. A nonsteroidal anti-inflammatory medicine (NSAID) is usually the treatment that has the worst prognosis. Distinct renal segments may experience varying degrees of kidney damage as the inflammation advances gradually. Kidney damage can occasionally become irreparable and affect one or both kidneys.
Immunosuppressive Therapy – Navigating the Immune System Rapids:
When our immune system turns into a wild river, immunosuppressive therapy acts as the guide, preventing it from veering off course. This explores how these therapies help maintain the delicate balance required for kidney health.
About the Creator
Enjoyed the story? Support the Creator.
Subscribe for free to receive all their stories in your feed. You could also pledge your support or give them a one-off tip, letting them know you appreciate their work.




Comments
There are no comments for this story
Be the first to respond and start the conversation.