Content warning
This story may contain sensitive material or discuss topics that some readers may find distressing. Reader discretion is advised. The views and opinions expressed in this story are those of the author and do not necessarily reflect the official policy or position of Vocal.
RENAL FIBROSIS
CAUSES, SYMPTOMS AND TREATMENT OPTIONS
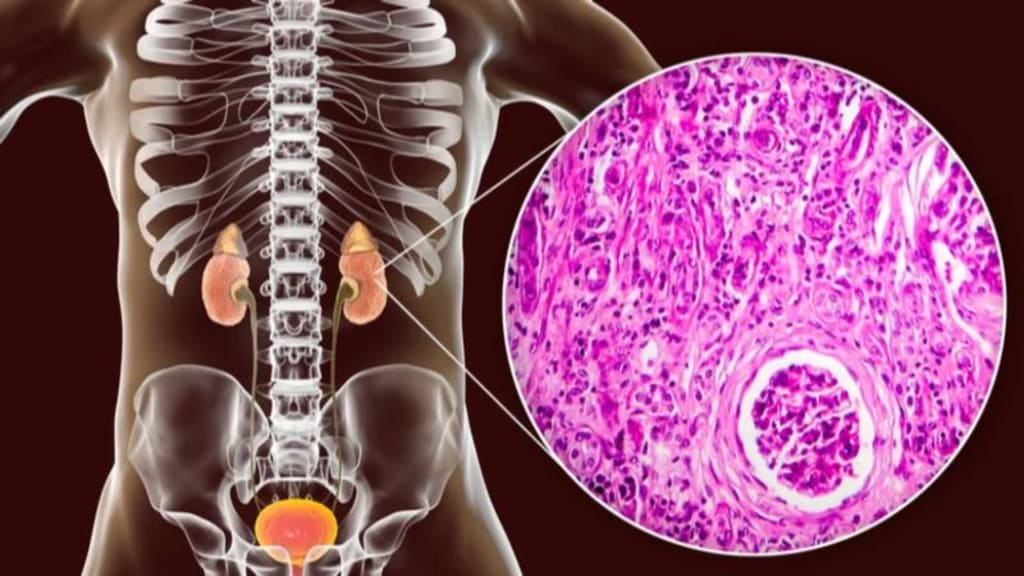
Renal fibrosis, also known as kidney fibrosis, is a pathological condition characterised by the excessive accumulation of extracellular matrix (ECM) proteins, particularly collagen, in the kidney tissue. This leads to fibrous or scar tissue forming in the renal parenchyma (functional tissue of the kidney). Renal fibrosis is a common feature of many chronic kidney diseases and represents the final common pathway in the progression of kidney damage.
Recognising the signs is imperative for early intervention. Reduced urine output, oedema, hypertension, fatigue, anaemia, and changes in urine appearance are key indicators. Fortunately, there are various treatment options available. These range from blood pressure management and dietary modifications to more advanced interventions such as dialysis or kidney transplantation in severe cases.
Early detection and a comprehensive, multidisciplinary approach are essential in managing renal fibrosis and improving the quality of life for affected individuals.
Causes of Renal Fibrosis
The causes of renal fibrosis include:
Chronic Kidney Disease (CKD): Chronic kidney disease is the most common underlying cause of renal fibrosis. Prolonged kidney damage, often due to conditions such as hypertension or diabetes, triggers a cascade of events leading to fibrotic renal tissue changes.
Inflammation and Immune Response: Inflammatory conditions, such as glomerulonephritis and autoimmune disorders such as lupus, can provoke an immune response that leads to fibrosis.
Toxic Exposures: Certain drugs, environmental toxins, and heavy metals can damage the kidneys and promote fibrosis.
Genetic Predisposition: Some individuals may have a genetic predisposition to develop renal fibrosis. Certain mutations can affect the way the kidneys handle stress and injury.
Glomerulonephritis: Inflammation of the glomeruli (filtration units) can result in kidney scarring.
Normal healthy glomeruli (left) with glomerulosclerosis (right). The scar tissue is shown in blueNormal healthy glomeruli (left) with glomerulosclerosis (right). The scar tissue is shown in blue
Infections: Certain infections, such as chronic pyelonephritis, can lead to kidney inflammation and fibrosis.
Normal kidney vs Chronic PyelonephritisNormal kidney vs Chronic Pyelonephritis
Autoimmune Disorders: Conditions such as lupus or vasculitis may cause kidney inflammation and fibrosis.
Obstruction: Persistent blockages in the urinary tract, such as kidney stones or tumours, can lead to back pressure and damage to kidney tissue, ultimately contributing to fibrosis.
Symptoms of Renal Fibrosis
Here are the symptoms of renal fibrosis:
Reduced Urine Output: A noticeable decrease in urine production, potentially leading to oliguria (very low urine output) or anuria (complete cessation of urine production).
Oedema: Swelling, especially in the lower extremities, due to fluid retention as the kidneys struggle to maintain fluid balance.
Hypertension: High blood pressure is a common symptom of renal fibrosis, often due to the kidney’s compromised ability to regulate blood pressure.
Fatigue and Weakness: The accumulation of waste products in the blood and electrolyte imbalances can lead to a general feeling of weakness and fatigue.
Anaemia: Kidneys produce a hormone called erythropoietin, which stimulates red blood cell production. When the kidneys are damaged, this can lead to anaemia.
Changes in Urine Appearance: Urine may appear foamy due to excess protein, or it may be discoloured, indicating the presence of blood or other abnormal substances.
Treatment Options For Renal Fibrosis
Treatment options include
Blood Pressure Management: Controlling blood pressure is crucial to slowing the progression of renal fibrosis. Medications such as angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) are often prescribed.
Dietary Modifications: A low-sodium, low-protein diet may be recommended to ease the kidney workload and manage fluid balance.
Diuretics: These medications help remove excess fluid and reduce oedema.
Treatment of Underlying Conditions: If renal fibrosis results from an underlying condition such as diabetes or autoimmune disease, managing that condition is paramount.
Dialysis: In advanced stages of renal fibrosis, when kidney function is severely impaired, hemodialysis or peritoneal dialysis may be necessary to perform the kidney’s filtering functions.
Dietary Changes: A dietitian may recommend dietary modifications, including reducing sodium, protein, and phosphorus intake, to ease the workload on the kidneys.
Hydration: Staying well-hydrated can help prevent kidney stones and reduce the risk of further kidney damage.
Kidney Transplant: In end-stage renal disease (ESRD) cases, a kidney transplant may be the best option for restoring kidney function.
Experimental Therapies: Ongoing research explores various approaches, including targeted medications to inhibit fibrosis-promoting pathways, stem cell therapies, and gene therapies.
About the Creator
Enjoyed the story? Support the Creator.
Subscribe for free to receive all their stories in your feed. You could also pledge your support or give them a one-off tip, letting them know you appreciate their work.





Comments
There are no comments for this story
Be the first to respond and start the conversation.