Content warning
This story may contain sensitive material or discuss topics that some readers may find distressing. Reader discretion is advised. The views and opinions expressed in this story are those of the author and do not necessarily reflect the official policy or position of Vocal.
Introduction
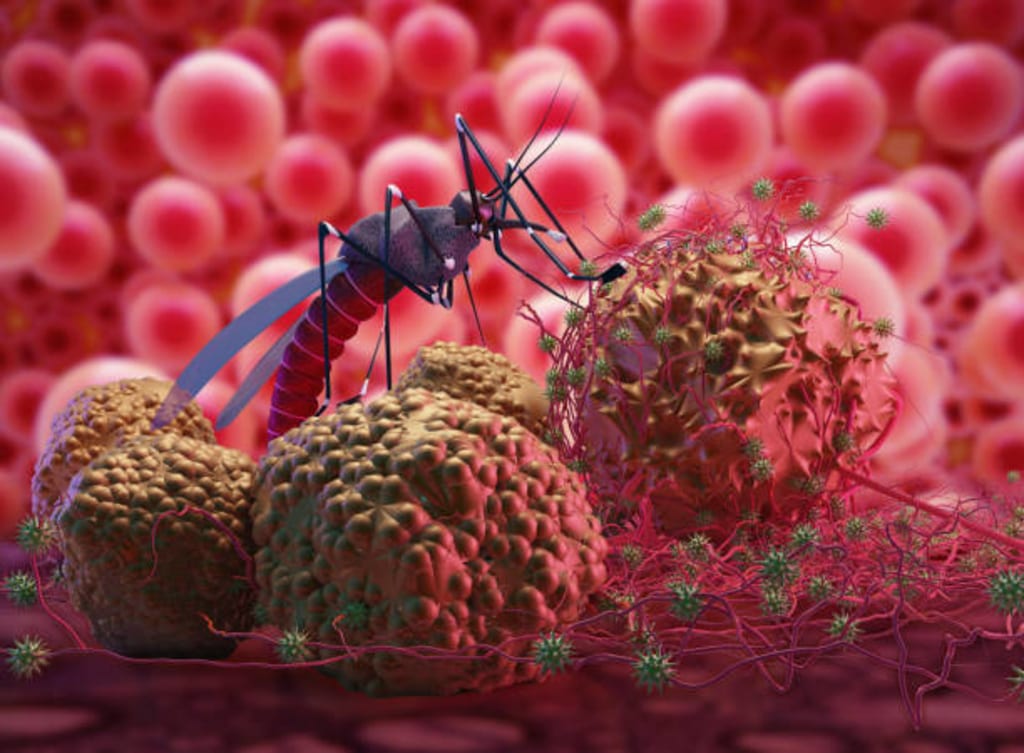
Malaria is an infectious disease spread by mosquitoes that affects both people and other animals. Serious malaria can strike some people more easily than others. Pregnant women, children under the age of 5, people with HIV/AIDS, and infants and young children are at high risk. Additional vulnerable populations include migrants, mobile populations, and travelers who enter areas with high rates of malaria transmission and who have not developed partial immunity from repeated exposure to the disease or who are not receiving chemo preventive medications. In places where malaria is common, some people will develop a partial immunity. Partial immunity never offers full protection, but it lowers the possibility that a malaria infection would result in serious illness. WHO presents all relevant information on Malaria Questions and answers? Malaria is a life-threatening disease primarily found in tropical countries the majority of malaria deaths in Africa therefore affect young children, whereas in regions with low immunity and limited transmission, all age groups are at danger. The risk of malaria is greatest in sub-Saharan Africa, where six nations—Nigeria (26.8%), the Democratic Republic of the Congo (12%), Uganda (5.4%), Mozambique (4.2%), Angola (3.4%), and Burkina Faso (3.4%)—accounted for more than half of all malaria deaths globally in 2020.
Clinical signs and Symptoms
The earliest signs of malaria often appear 10 to 15 days after being bitten by an infected mosquito. The classic symptoms of malaria include fever, headache, and chills, though they may be mild and difficult to identify. In locations where malaria is endemic, those with limited immunity may contract the disease yet not show any signs of illness (asymptomatic infections). WHO advises rapid diagnosis for everyone with malaria suspicions. Malaria caused by Plasmodium falciparum can develop to serious sickness and death if it is not treated within 24 hours. Adults with severe malaria can experience multi-organ failure, whereas children with severe anaemia, respiratory distress, or cerebral malaria are usually affected. Several Plasmodium species can cause human malaria, which can lead to serious illness and occasionally even life-threatening disease. Using tests that identify the presence of the disease-causing parasites, malaria can be identified. Rapid diagnostic tests and microscopic analysis of blood smears are the 2 primary categories of tests. Diagnostic tests allow medical professionals to differentiate between malaria and other causes of febrile diseases, facilitating the right course of treatment.
Diagnosis and Treatment
The first and only vaccine that has shown it can dramatically lower malaria in young children living in areas with a moderate-to-high malaria transmission rate is RTS,S/AS01 (RTS,S). It combats Plasmodium falciparum, the most dangerous malaria parasite in the world and the most common in Africa. WHO approved the RTS,S vaccine in October 2021 for kids residing in regions with moderate to high malaria transmission rates. The entire body of RTS,S evidence, including the outcomes of the ongoing pilot program, served as the basis for the recommendation. Quinine, the first drug used to treat malaria, was made from Cinchona calisaya tree bark. William Henry Perkins made the first attempt at synthesizing quinine in 1856, but it wasn't until 1944 that the process was successful.
Prevention and Control
Malaria is a sickness that can be avoided.
1. Measures for vector control. The primary strategy for preventing malaria and reducing transmission is vector control. Insecticide-treated bed nets, which protect people from bites while they sleep and kill mosquitoes as they try to feed, and indoor residual spraying, which involves applying an insecticide to surfaces where mosquitoes tend to rest, such as internal walls, eaves, and ceilings of homes and other domestic structures, are two effective vector control methods for people living in malaria-endemic countries. The most useful vector control strategy for travellers is the use of an insecticide-treated net. The World Health Organization keeps a list of vector control products that have been evaluated for their quality, safety, and efficacy.
2. 2. Chemoprophylaxis and chemo preventive treatments. Certain antimalarial medications can be used to prevent the disease even if they are intended to treat patients who have malaria. The intermittent preventive treatment of malaria in pregnancy, the intermittent preventive treatment of malaria in infants, and the seasonal malaria chemoprevention for children under the age of five is the current WHO-recommended malaria chemo preventive therapies for people living in endemic areas. When entering a region where malaria is endemic, travellers are also given chemoprophylaxis medications, which are very effective when used in conjunction with insecticide-treated nets.
Conclusion
A malaria-free world is the goal shared by WHO and the international malaria community. Countries will gradually attain this aim by eradicating malaria from their national borders and putting in place practical controls to stop transmission from starting up again. The locations of malaria-endemic nations on the road to eradication vary. The effectiveness of the national healthcare system, the level of investment made in malaria eradication plans, and other elements, such as biological determinants, the environment, and the social, demographic, political, and economic realities of a specific country, all influence the rate of progress. To be eligible for the WHO certification of malaria elimination, a country must have at least three years in a row with no indigenous cases of malaria (a case contracted locally with no proof of importation from another endemic country). Since 2000, the accreditation has been granted to eleven nations, most notably China and El Salvador. Since 2015, nine nations—the Maldives (2015), Sri Lanka (2016), Kyrgyzstan (2016), Paraguay (2018), Uzbekistan (2018), Argentina (2019), Algeria (2019), El Salvador (2021), and China—have received the WHO Director-certification General's that they are malaria-free (2021).
About the Creator
Enjoyed the story? Support the Creator.
Subscribe for free to receive all their stories in your feed. You could also pledge your support or give them a one-off tip, letting them know you appreciate their work.




Comments
Rida Fatima is not accepting comments at the moment
Want to show your support? Send them a one-off tip.