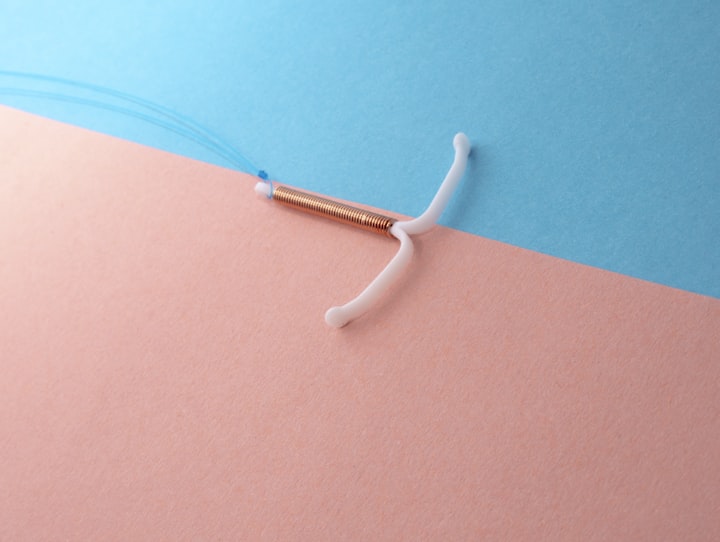
IUD Insertion Pain & Your Options
Putting the power back into your hands
Over the last year (and likely even before that), there’s been more and more discussion around the insertion of IUDs for birth control and the surfacing of lived experiences. To the distress of many, it has not been positive.
I will disclose that I’ve never had an IUD – in fact, I’ve never used a birth control medication in my lifetime thus far (and for this reason I don’t ever use my lived experiences when providing care to my patients. It would be unethical – anecdotal evidence is great, but it is not where best practices are founded). My knowledge comes from my independent research of best practices in order to stay up to date and best serve my patients.
IUDs are a wonderful medical tool for birth control access. They’re long-acting, safe to use and can provide the freedom that people deserve to decide when and if they have children. What becomes unfortunate is the way informed consent is gathered for IUD insertion. It’s important to have all the information you need to make the best choice for your body, and while it isn’t typically in a providers interest to harm you, when clinics are understaffed, providers are overworked or have conflicts that interfere with their decision making and emotional awareness, people get hurt.
As a super basic intro this, here’s how an IUD is inserted:
1. A speculum is inserted into the vagina – in the exact same way it is done for an internal pelvic exam or pap smear. A lubricant on the speculum is typically used to help this insertion be more comfortable. Once inserted, the speculum is gently opened to allow your provider to visualize your cervix and access it.
2. A tool called a tenaculum is used to hold the cervix in place for cleaning and IUD insertion. It has two needle-like tips that grab on to the cervix – it has to pierce the tissue to hold it, and this is when you may notice pinching or pain. There can be spotting after insertion due to this.
3. A special tool (called a sound) that holds the IUD itself is inserted into the cervix. Markings are present on the tool in order to measure the length and direction of the cervical canal and uterus.
4. The IUD is pushed out of the tool and into place. The tools are removed and your provider will trim the strings of the IUD (you can check these at a later time to ensure your IUD is still in place).
It’s common for a provider to recommend taking some Advil or Tylenol before your appointment so any pain or pinching is lessened. It’s very similar to how I prepared for my first tattoo!
Here’s where it can get a bit sticky: ibuprofen (Advil) has not been shown to be effective in reducing pain with IUD insertion. And unlike what some providers may suggest, the cervix has LOTS of nerve endings and CAN feel pain, and the experience of pain is NOT different between white people and BIPOC (reproductive health research has some really racist origins, folks).
So what does the research show?
Lidocaine-prilocaine cream (otherwise known as LPC) has been found to reduce the pain of tenaculum use by about 24% and IUD insertion by 28% (Whitworth, Neher, Safranek 2020). Some providers may give vaginal misoprostol to soften the cervix and then use a lidocaine solution with a bit of success, but this drops down to less than 20%. Pretreating with lidocaine gel, a lower dose of oral misoprostol and ibuprofen hasn’t been found to be effective in reducing pain. It’s also suggested that a paracervical block (think like an epidural) may also be helpful but we need more research to identify this clearly.
If you’re planning an IUD insertion, it’s important to ask your provider what they can offer to you in terms of pain management – your experiences are real and valid, and you deserve the highest quality of care.
- Can the provider offer lidocaine in office? If not, why not?
- Do you have the option for a paracervical block, or even general anesthetic? (Some hospitals do offer this, especially for young individuals receiving their first IUD)
- Can they review the process of insertion both prior to the appointment and before they begin the insertion? Informed consent can be withdrawn at any time.
- Will the provider stop the insertion if you vocalize pain? If not, find a new provider ASAP.
- What are your other birth control options that aren’t inserted vaginally? Think Nexplanon, Depo-provera, NuvaRing or Evra.
- What should you expect after the insertion in terms of pain and other symptoms? When is it a red flag to return to office? It’s suggested to bring a support person with you, as it’s possible you might not be able to drive.
Reproductive rights are having unbarred and inclusive access to the decision if, when and how you choose to get pregnant. Your reproductive health care should reflect that.
About the Creator
Emily the Period RD
I help people with periods navigate menstrual health education & wellness with a healthy serving of sass (and not an ounce of nutrition pseudoscience).






Comments
There are no comments for this story
Be the first to respond and start the conversation.