VA surgery delay leaves caregiver, mother dead
Media attention has inspired reforms at VA

An earlier version of this article appeared on News Break.
Some encouraging news published in JAMA Surgery came too late for my former next-door neighbors in Rock Island, Ill.
That’s because Monica, a Scottish immigrant, and her son, Paul, both are now dead.
Paul, who was in his early fifties, cared for his mom in the house they rented next door to me. Like myself, Paul at times became overwhelmed by his mother, who had dementia like my dad.
Monica appeared not as bad as my dad, at least at first. But Monica was about 90 years old.
When Paul began to lose a lot of weight, I asked him what was going on. He told me he had not been feeling well but could not get into the VA right away due to long wait times.
Finally, he got in and they discovered he had a cancerous tumor in his colon. They scheduled the surgery for several weeks out.
By the time they opened Paul up, he was full of cancer. He died in weeks. I remember him telling me he was going to die "but don't tell my mother." He offered me all of his beer in the house because he could not drink it. I was sober and turned down the beer.
Monica, her heart broken by the death of her only child, began to exhibit worsening dementia. Daily home care wasn’t enough.
Monica was coaxed from her home by police one day never to return.
After a short stint in a hospital where unruly elderly people are heavily medicated and made “manageable,” she discharged into a nursing home and died.
She died alone, at the troubled, county-owned nursing home. I tried to call and inquire about her a couple of times but got nowhere.
A sad story. She became a ward of the state after Paul died; the state got everything she owned to pay the nursing home bills.
The house sat unrented for months with much of their belongings still there.
Red tape rolled out by the state meant the landlord could not touch her belongings. They had seized her assets. He had no way to rent the property for several months.
Media attention inspires VA reforms
The study released in JAMA Surgery shows how reforms put in place at a VA pilot location in Indianapolis drastically reduced delays.
Using the Richard L. Roudebush Veterans Affairs Medical Center as a test site, “Multidisciplinary teams identified systemic inefficiencies and strategies to improve interdepartmental and patient communication to reduce canceled consultations and cases, diagnostic rework, and no-shows,” according to JAMA.
“High-priority triage with enhanced operating room flexibility was instituted to reduce scheduling wait times. General surgery department pilot projects were then implemented mid-fiscal year 2013.”
Wait times were shaved by 33 days in fiscal year 2012 to 12 days by fiscal year 2014. The number of patients operated on increased from 931 in fiscal year 2012 to 1072 in fiscal year 2014.
“This study demonstrated a significant reduction in patient wait times for surgical procedures and an improvement in access in the clinical and operative settings when implementing lean processes,” the authors wrote.
“The improvement gained was noted over multiple areas and seen during the implementation of new technologies. The changes in the measured outcome categories occurred early, and the differences were sustained across the entire observation period.”
The authors reported that a “systems redesign” involving “personnel, clinicians and surgical staff to reduce systemic inefficiencies” could work throughout the VA.
In an accompanying editorial, Drs. June Ray Juliet and Seth A. Spector of Miami wrote, “Widespread negative media attention targeting patient access and wait times at the U.S. Department of Veterans Affairs institutions has prompted evidence-based reform to improve health care access and delivery.
“The stakes are high, and process, organization, and infrastructure must be reformed to ensure that health care delivery, research, education, and training proceed at the highest standard,” the editorial concludes.
Hospice in Scotland celebrates life while managing pain
Monica was cremated and a small service was held at a later date. I attended the service, which was held across the street from Monica and I's homes at St. Pius X Catholic Church, where Monica was a member. It was my first Catholic funeral.
Ironically, around the time Monica died I reviewed a film about a hospice in Scotland, Monica’s homeland.
At Strathcarron, patients not only stay in their homes for as long as possible, but once a week they attend “day hospice” and truly celebrate life.
They sing regularly, and with gusto along with other hospice patients and staff.
The documentary “Seven Songs for a Long Life” debuted at the South by Southwest (SXSW) film festival in Austin, Texas.
You can learn more about the film and watch a trailer by clicking here.
The cast of characters is delightful. The film’s cinematography is especially meaningful. It captures the beauty of the hospice, its people, and the Scottish countryside itself.
Day hospice model relatively unique to Scotland
Amy Hardie, director of the film, told me there is no “day care” hospice model in the U.S. The hospital in Scotland is funded in part by the U.K. National Health Service but still needs to raise a significant amount of money each year to stay open. It’s not easy in a working-class area.
But the development director, a key cast member named Jim Brown, manages to pull it off by raising the needed 3.9 million pounds every year.
“It means that patients can stay at home but know that each week they are coming in for a day where they will have expert medical attention by people they have got to know over months and often years,” Hardie told me in an email interview.
“It is also a day where they meet with the same other patients who have a terminal illness, who are confronting their own mortality, but are often able to be kept pain free and mobile.
“These patients are hungry for life – they may know they are going to die of their disease, but there is life to be lived right up to the end, and hospice care is about helping them to make that life as fulfilling as possible – hence my role as film-maker in residence.
“No-one wants to be defined as a patient – singing was a potent way for the patients to show that they were more than patients …. Each song shows how very alive they are, right up to the moment of death.”
About the Creator
David Heitz
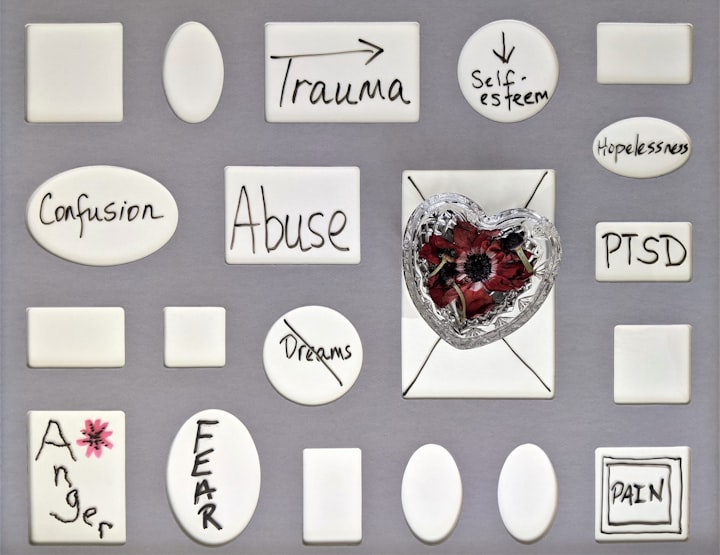
I am a journalist with more than 30 years' experience. Here at Vocal, I write mainly for Potent, Vocal's cannabis magazine. I have a PTSD diagnosis and a medical cannabis card. I have lived in a penthouse and also experienced homelessness.





Comments
There are no comments for this story
Be the first to respond and start the conversation.