When Temperature Matters: Raynaud's Phenomenon Uncovered
Understanding the Complexities of a Vascular Condition

Raynaud's phenomenon (RP) is a fascinating condition that causes blood vessels, predominantly in the fingers and toes, to constrict excessively in response to cold or emotional stress. This intricate process is governed by the body's natural ability to regulate its internal temperature and maintain a stable core body temperature.
Under normal circumstances, blood vessels supplying the skin constrict, or narrow, in cold temperatures. This vasoconstriction helps conserve heat by reducing blood flow to the skin, ensuring a stable core temperature. Conversely, in warm conditions, blood vessels dilate, or widen, increasing blood flow to the skin surface and allowing heat to dissipate, thus preventing the core body temperature from reaching dangerous levels.
Thermoregulatory blood vessels are primarily controlled by the sympathetic nervous system, which is also responsible for our stress response. This explains why both cold temperatures and emotional stress can trigger vasoconstriction, leading to cold fingers and toes.
However, individuals with Raynaud's phenomenon experience altered or defective vasoconstriction mechanisms. Their blood vessels constrict excessively in response to cold or emotional stress, resulting in a Raynaud's attack. This event is characterized by three distinct phases, each marked by skin color changes. Initially, severe vasoconstriction restricts blood flow to the affected areas, causing the skin to feel cold and appear white.
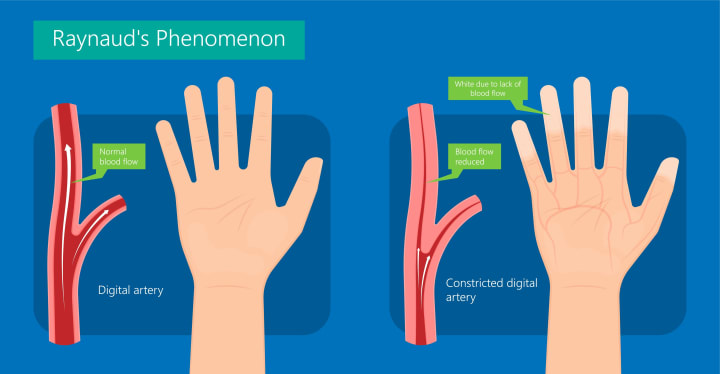
This pallor is due to an almost complete lack of blood flow. Subsequently, the skin typically develops a purplish-blue hue (acrocyanosis) as blood flow through the skin is reduced. Finally, when the blood vessel fully recovers and dilates, blood flow resumes, and the skin may flush to a vivid pink or red color.

Explore the complexities of Raynaud's phenomenon with us as we delve into the intricate relationship between blood vessels, temperature, and emotions, and learn how these factors intertwine to impact the lives of those affected by this condition.
RAYNAUD'S PHENOMENON RISK FACTORS
It is estimated that Raynaud phenomenon (RP) affects 3 to 5 percent of the general population.
Primary disease
Primary RP occurs when individuals experience RP without an associated disease. The root cause of blood vessel sensitivity to cold in primary RP remains unclear. However, there is evidence suggesting that it may be a familial trait, pointing to the possible involvement of one or more genes that regulate skin blood flow.

Interestingly, primary RP is responsible for the majority of cases and is more prevalent among females, younger individuals (those under 30), and family members of people with RP. The good news is that most people with primary RP do not have an underlying medical issue. While their symptoms can be bothersome, they are generally not severe and are unlikely to result in long-term damage. Those with primary RP are more likely than people with secondary RP to successfully manage their condition with simple, non-pharmaceutical interventions.
Over time, primary RP often improves as individuals learn to anticipate and prepare for cold temperatures and emotional triggers. Join us as we delve into the fascinating world of primary Raynaud's phenomenon, exploring its origins, manifestations, and the ways in which those affected can adapt to this enigmatic condition.
Secondary disease
Secondary Raynaud's phenomenon (RP) affects individuals who have an underlying disease or a specific cause for their RP symptoms. There are several known origins of secondary RP, with autoimmune rheumatic diseases, such as scleroderma or systemic lupus erythematosus, being a common source. These diseases trigger secondary injuries that alter blood vessels, consequently impacting their response to stimuli like cold temperatures and stress.
Managing secondary RP can be more challenging than primary RP due to its connection to an underlying condition that can physically damage blood vessels. As a result, people with secondary RP are more likely to require medications to alleviate their symptoms.
RAYNAUD'S PHENOMENON CAUSES
Raynaud's attacks most commonly affect blood vessels in the fingers, but can also influence other areas of the body. During a typical attack, fingers or toes may suddenly feel cold as blood vessels constrict, leading to significant skin color changes. These changes can manifest as pale "white attacks" or purple-blue "blue attacks". Attacks often begin in a single finger before spreading to other digits in both hands, with the index, middle, and ring fingers being most commonly impacted. Interestingly, the thumb is frequently spared.
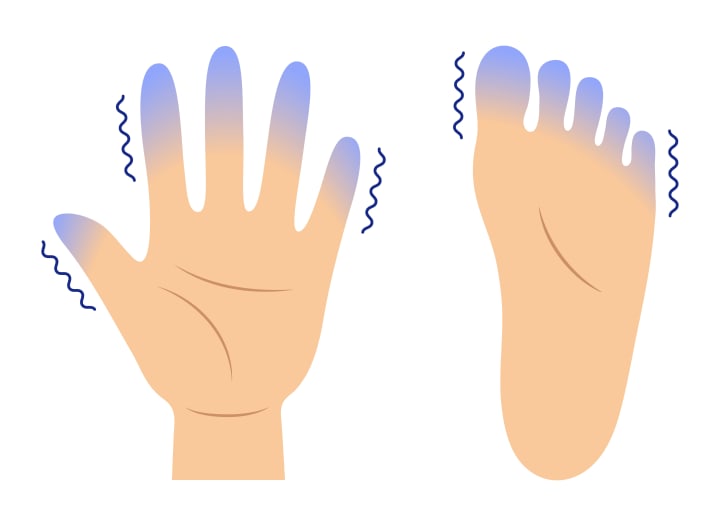
These attacks can induce discomfort, such as a "pins and needles" sensation, aching, numbness, or clumsiness in the affected hand(s). True pain is more common in secondary RP, resulting from prolonged blood flow loss to tissues.
Blood vessels supplying the skin of the ears, nose, face, knees, and nipples can also be affected, with skin in these areas turning pale or bluish after cold exposure. In rare instances, the tongue may be involved, and temporary mottling (bluish discoloration) of the skin on the arms and legs might appear. Attacks affecting the toes are also common, though reported less frequently.
Symptoms of RP typically subside once the provoking factor (cold or stress) is removed. Discoloration resolves after 15 to 20 minutes of rewarming, and as normal blood flow resumes, the skin may "blush" or turn pink. Mild discomfort may be experienced during the recovery phase.
In severe cases of secondary RP, blood flow may not recover even after the provoking factor or cold is removed, due to underlying blood vessel damage or irreversible structural changes such as vessel blockage. This can lead to pain and skin ulceration (usually on finger and toe tips). In extreme cases, deeper tissue injury may occur, potentially resulting in the loss of finger tips in individuals with secondary vascular diseases causing RP.
RAYNAUD'S PHENOMENON DIAGNOSIS
The diagnosis of RP largely hinges on a person's description of a typical attack following exposure to cold temperatures. By asking targeted questions, a healthcare provider can often determine whether RP or another more common condition is causing cold hands or feet. It is crucial to undergo a thorough evaluation by a healthcare professional to ascertain if RP is indeed occurring and identify the underlying cause of the condition.
This diagnostic process entails a comprehensive history and physical examination, as well as laboratory testing, which may include blood tests and, occasionally, specialized studies of blood vessels and their function.
RAYNAUD'S PHENOMENON TREATMENT
Managing RP can be improved with a combination of simple lifestyle changes and, when necessary, medication to control symptoms. Discover the various strategies and measures that can help reduce the frequency of RP attacks, promoting a more comfortable and stress-free life for those affected.
Combat Sudden Cold Exposure: Stay warm and prevent rapid temperature changes, cold drafts, and damp conditions. Dress warmly, wear layered clothing like thermal underwear, put on a hat, and use mittens or gloves to keep extremities warm.
End an Attack: Techniques to halt an attack include placing hands under warm water or in a warm spot (such as the armpits) and swinging arms in a windmill-like pattern.
Kick the Habit: Avoid smoking, as nicotine and other cigarette chemicals can constrict blood vessels and worsen RP symptoms.
Steer Clear of Vasoconstricting Medications: Medications that cause blood vessel narrowing, such as certain decongestants, amphetamines, diet pills, migraine remedies, herbs, and attention deficit disorder (ADD) medications, should be avoided.
Embrace Stress Reduction: Incorporate relaxation techniques and stress reduction strategies to minimize anxiety and keep RP symptoms in check.
Medicine
When lifestyle changes and self-care measures aren't enough to manage RP symptoms, medication may be the next course of action. Medications for RP work by dilating the thermoregulatory blood vessels, thereby improving blood flow. Calcium channel blockers are the most commonly prescribed medications, offering daily relief by reducing both the frequency and severity of Raynaud's attacks. In addition to calcium channel blockers, several other medications can be used to manage RP symptoms. Each medication targets different aspects of the condition, and a healthcare provider may recommend one or more of these drugs based on an individual's unique needs and circumstances. Some alternative medications for RP include:
1. Alpha-blockers: These medications counteract the effects of norepinephrine, a hormone that constricts blood vessels. By blocking its action, alpha-blockers can help improve blood flow. Examples include prazosin and doxazosin.
2. Vasodilators: These drugs directly help widen blood vessels, promoting better blood flow to the extremities. Examples include nitroglycerin cream and sildenafil (Viagra), which are both known for their vasodilating properties.
3. Prostaglandins: Prostaglandins like iloprost can help dilate blood vessels and prevent platelet aggregation, which can improve blood flow in individuals with severe RP symptoms. These medications are typically administered intravenously.
4. Angiotensin II receptor blockers (ARBs): These medications, such as losartan, can help relax blood vessels by blocking the action of angiotensin II, a hormone that narrows blood vessels.
5. Selective serotonin reuptake inhibitors (SSRIs): Some studies suggest that SSRIs, a class of antidepressants, may help improve RP symptoms by enhancing blood flow. Examples include fluoxetine and sertraline.
6. Topical treatments: In some cases, creams or gels containing vasodilating agents, like nitroglycerin, can be applied directly to the skin to alleviate symptoms.
It is essential to consult a healthcare professional to determine the most appropriate medication and treatment plan for managing Raynaud's phenomenon based on individual needs and medical history.
Secondary Raynaud's phenomenon
For individuals with secondary RP, more aggressive treatment may be necessary to manage symptoms and prevent skin injury on fingers and toes. Medication responsiveness can vary greatly in secondary RP cases, depending on the underlying cause and severity of blood vessel damage. Addressing the root cause, such as discontinuing a medication responsible for vasoconstriction, is a top priority.
Beyond calcium channel blockers, several alternative medications have been studied for those who do not respond to conventional treatments. These options include topical nitrates (nitroglycerin), phosphodiesterase inhibitors (sildenafil), and prostaglandins (prostacyclin). Additionally, botulinum toxin (Botox) injections at the base of the fingers have shown potential, but more research is needed to confirm their efficacy for RP.
In certain cases, hospitalization may be required if an RP attack does not resolve and blood flow is severely compromised, putting a finger or toe at risk. Treatment in such situations involves additional medications to dilate blood vessels, improve blood flow, and prevent tissue damage or ulcerations. In some instances, surgery may be employed to sever nerves at the finger base that trigger vasoconstriction or repair a blocked blood vessel supplying the affected area.
In rare cases, treatments may fail to reverse vasoconstriction, leading to skin ulceration. If all other interventions have been exhausted and deep tissue damage has occurred due to blood flow deprivation, surgical amputation of the affected finger or toe may become necessary.
About the Creator
Mohammad Barbati
Mohammad E. Barbati, MD, FEBVS, is a consultant vascular and endovascular surgeon at University Hospital RWTH Aachen. To date, he has authored several scientific publications and books regarding vascular and venous diseases.






Comments
There are no comments for this story
Be the first to respond and start the conversation.