The Strangling Ligament
Understanding Median Arcuate Ligament Syndrome
Today, we're going to delve into the fascinating world of ligaments, and more specifically, the star of our show: the Median Arcuate Ligament (MAL). Buckle up and let's unravel the mysteries of Median Arcuate Ligament Syndrome (MALS) together!
The Tale of the Tight Hug: What is Median Arcuate Ligament Syndrome?
Once upon a time, there was a ligament who loved to hug. The Median Arcuate Ligament, located in our abdominal cavity, is a fibrous arch that connects the diaphragm's crura (the muscle's tendons) on either side of the aorta, the body's main artery. Now, a hug is usually a warm and fuzzy thing, but in the case of MALS, our little ligament is hugging a bit too tight.


MALS occurs when the MAL compresses the celiac artery, reducing blood flow to the stomach, liver, and spleen. As a result, a bevy of symptoms can arise, including chronic abdominal pain, nausea, vomiting, and weight loss. MALS is a rare condition, often misdiagnosed or overlooked, but fear not! We're here to shed some light on it.

The Whodunit of Abdominal Pain: Diagnosing MALS
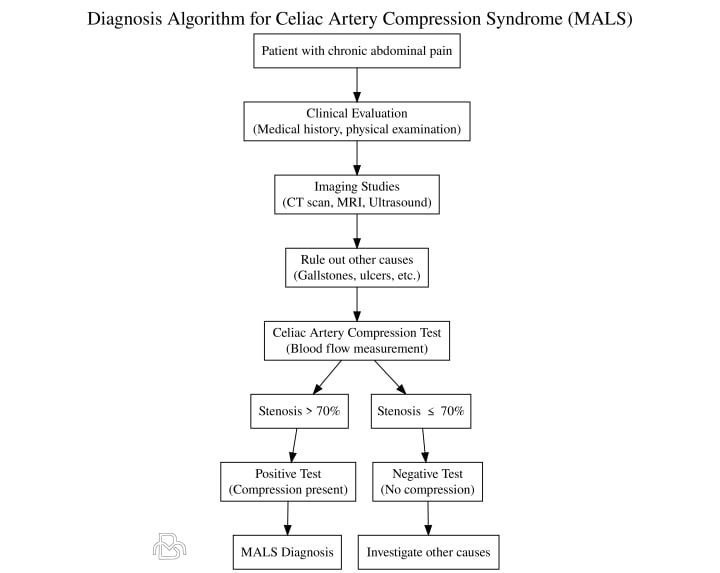
Picture this: you're a detective faced with a case of unexplained abdominal pain. You sift through the clues, eliminating suspects like gallstones and ulcers, but you're left with a lingering mystery. Enter MALS, the elusive culprit that often flies under the radar.

Diagnosing MALS can be a challenge. Doctors typically rely on a combination of imaging studies, such as CT scans, MRIs, and ultrasounds, as well as a patient's medical history and symptoms. One diagnostic tool, the "celiac artery compression test," involves measuring blood flow in the celiac artery before and after a deep breath. If the blood flow decreases significantly during the breath, it may indicate MALS.
A Breath of Clarity: Inspiratory and Expiratory Vascular Imaging in MALS Diagnosis
A Breath of Clarity: The Power of Inspiratory Vascular Imaging
Imagine you're a professional deep-sea diver, and your mission is to uncover the secrets of the ocean floor. You take a deep breath, and as you descend, the water pressure increases, revealing hidden treasures and underwater phenomena. This is much like what happens during inspiratory vascular imaging, a diagnostic tool used in MALS cases.

Inspiratory vascular imaging involves capturing images of the celiac artery and surrounding structures while the patient takes a deep breath. This deep breath increases pressure in the abdominal cavity, which can accentuate the compression caused by the MAL. By comparing these images to those taken during normal breathing, doctors can detect any significant changes in blood flow and visualize the source of the problem.
Exhaling the Mystery Away: The Role of Expiratory Vascular Imaging
Now, picture yourself as a master yogi, expertly guiding your students through a series of breathing exercises. As they exhale, they release tension and stress, allowing for a clearer understanding of their inner selves. Expiratory vascular imaging works in a similar way, providing valuable insights into the nature of MALS.
During expiratory vascular imaging, patients are asked to exhale fully and hold their breath. This maneuver allows doctors to examine the celiac artery and its surroundings in a different physiological state. In some cases, this can help confirm the diagnosis of MALS or rule out other potential causes of the patient's symptoms.
By incorporating both inspiratory and expiratory vascular imaging into the diagnostic process, healthcare professionals can gain a comprehensive understanding of the celiac artery's dynamics in MALS cases. Together, these tools act as underwater flashlights and calming exhales, illuminating the mysteries of the Median Arcuate Ligament and guiding patients toward the most appropriate treatment options.
The Unlikely Hero: Treatment Options for MALS
In the realm of MALS therapy, there's an unlikely hero: surgery. When conservative treatments like pain management and dietary changes fall short, surgical intervention may be the key to unlocking relief for MALS patients.

The most common surgical option is the Median Arcuate Ligament Release (MALR). During this procedure, surgeons carefully cut the ligament to free the celiac artery from its tight embrace. This allows blood flow to return to normal, alleviating the patient's symptoms. Another approach is the Celiac Artery Bypass, where surgeons create a new pathway for blood flow to bypass the compressed artery.
The Rollercoaster of Recovery: Life After Surgery
The road to recovery after MALS surgery can be a rollercoaster. Initially, many patients experience significant relief from their symptoms. However, it's not uncommon for some discomfort to persist or even new symptoms to emerge.
Recovery time varies, but most patients can resume normal activities within a few weeks. It's essential to follow your doctor's advice, including any prescribed medications and physical therapy recommendations. Remember, it's a marathon, not a sprint, and patience is key to a successful recovery.
The Mysterious Disappearance: When MALS Symptoms Vanish
In some cases, MALS symptoms can disappear on their own, much like a magician's disappearing act. While it's not entirely understood why this happens, some theories point to changes in body position, weight loss, or even spontaneous ligament stretching.
Although it's tempting to embrace the vanishing act, patients should still consult their healthcare providers. A thorough evaluation can rule out other potential causes and ensure that MALS is indeed the source of their symptoms.
The Case of the Copycat: MALS Mimics
MALS has a few doppelgangers in the abdominal pain world. Conditions like gastroparesis, functional dyspepsia, and chronic mesenteric ischemia can present with similar symptoms, making it crucial to rule them out before identifying MALS as the cause.
The importance of a thorough medical evaluation cannot be overstated. By differentiating MALS from its mimics, healthcare providers can ensure patients receive the appropriate treatment and avoid unnecessary interventions.
Some common misdiagnoses of MALS include:
Gastroesophageal reflux disease (GERD): MALS can cause abdominal pain and discomfort that may be mistaken for GERD, a more common condition in which stomach acid irritates the esophagus.
Irritable bowel syndrome (IBS): MALS patients often experience abdominal pain, bloating, and changes in bowel habits, which can be similar to the symptoms of IBS.
Functional dyspepsia: This condition is characterized by chronic or recurrent pain in the upper abdomen, which can be similar to the pain experienced by MALS patients.
Peptic ulcer disease: Peptic ulcers, which are sores in the lining of the stomach or duodenum, can cause abdominal pain similar to that experienced in MALS.
Gallbladder disease: MALS symptoms can be mistaken for gallbladder issues, such as gallstones, which can also cause abdominal pain and discomfort.
Pancreatitis: Inflammation of the pancreas can cause abdominal pain and other symptoms that may be mistaken for MALS.
Splanchnic artery syndrome: This rare condition occurs when blood flow to the digestive organs is reduced, leading to symptoms that can be similar to MALS.
Pelvic congestion syndrome: This condition, which involves the pooling of blood in pelvic veins, can cause chronic pelvic pain that may be mistaken for MALS.
Nutcracker syndrome: This rare vascular disorder results from the compression of the left renal vein and can cause symptoms similar to MALS, including abdominal pain.
Endometriosis: A condition in which endometrial tissue grows outside the uterus, endometriosis can cause pelvic pain and other symptoms that may be misinterpreted as MALS.
The Support Squad: Finding Help and Community
No one should face the challenges of MALS alone. A crucial aspect of coping with this rare condition is finding support and community. Online forums, social media groups, and patient advocacy organizations can be invaluable resources for MALS patients and their families.

Connecting with others who share similar experiences can provide emotional support, practical advice, and a sense of belonging. Additionally, these communities can help raise awareness about MALS, promote research, and advocate for better diagnostic and treatment options.
The Plot Twist: MALS in Children and Young Adults
In a surprising turn of events, MALS doesn't only affect adults. Although it's more commonly diagnosed in middle-aged women, MALS can also occur in children and young adults. The presentation of symptoms and diagnostic process remains similar, but treatment options may vary based on age and individual circumstances.

Early intervention is key when addressing MALS in younger patients. A multidisciplinary approach involving pediatric specialists, nutritionists, and mental health professionals can help ensure the best possible outcome for children and young adults with MALS.
The Silver Lining: Success Stories and Hope
Every cloud has a silver lining, and MALS is no exception. Many patients have found relief from their symptoms through surgery or other treatments, reclaiming their quality of life. These success stories offer hope to those still struggling with the challenges of MALS.
It's important to remember that each patient's journey is unique. Some may find relief quickly, while others take a more winding path to recovery. Regardless, staying positive and persevering can make all the difference when navigating the world of MALS.
The Final Act: Raising Awareness and Expanding Knowledge
As our adventure draws to a close, it's crucial to recognize the power of knowledge and awareness. By understanding MALS and sharing our newfound wisdom, we can help those affected by this rare condition find the answers they seek.
As research progresses and the medical community becomes more familiar with MALS, we can hope for improved diagnostic tools, more effective treatments, and a brighter future for patients. And with that, our gutsy ligament's story comes to an end - but the quest for knowledge never does.
About the Creator
Mohammad Barbati
Mohammad E. Barbati, MD, FEBVS, is a consultant vascular and endovascular surgeon at University Hospital RWTH Aachen. To date, he has authored several scientific publications and books regarding vascular and venous diseases.






Comments
There are no comments for this story
Be the first to respond and start the conversation.