Polyenes, Nystatin and mode of action of different antifungal drugs.
Introduction of different antifungal drugs.
Polyenes
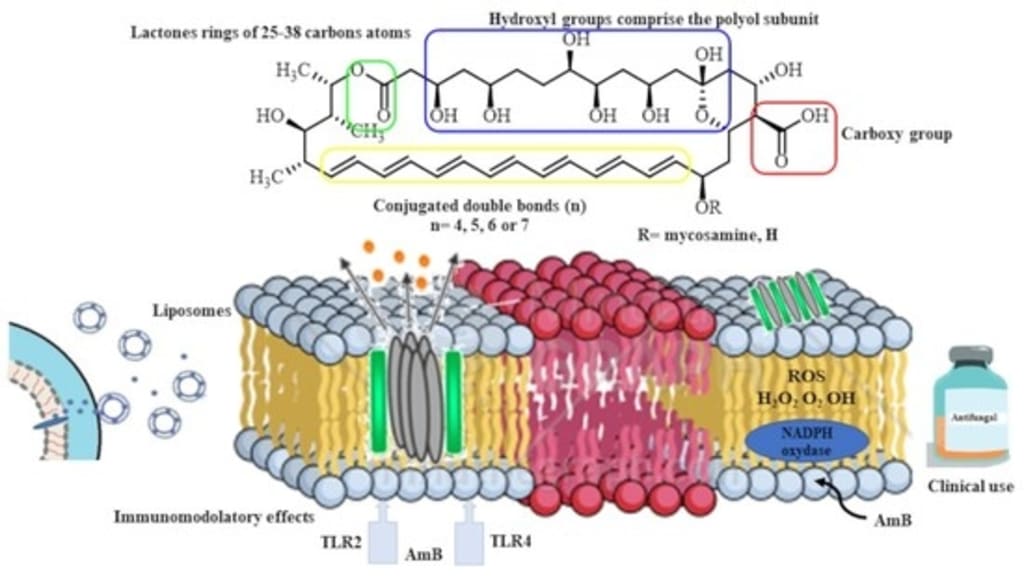
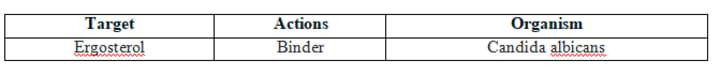
Nystatin and amphotericin are polyenes, which are active against some fungi but have little action on mammalian cells and no action on bacteria. They bind to cell membranes and interfere with permeability and transport functions as well as they kill fungal cells by making the fungal cell wall more porous, which makes the fungal cell prone to burst.
Some examples of polyene antifungals are:
Amphotericin B: It is a polyene antibiotic prototype that has a high affinity for the ergosterol present in fungal cell membranes. After combining with the membrane and being inserted into it, a number of molecules align themselves to form the micropore.
Nystatin:
Nystatin, which is derived from the noursei plant, shares some characteristics and an antifungal effect with Amphotericin B.
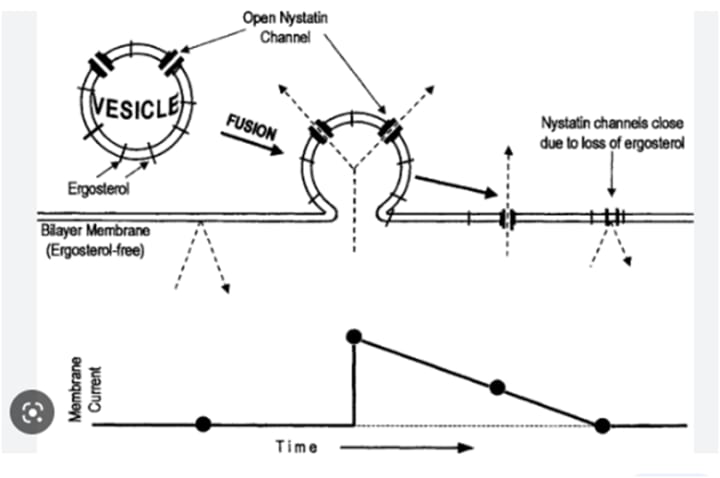
It creates holes by adhering to the membrane of fungal cells (ergosterol).
This changes permeability and transport, which leads to cell death.
The macrocyclic rings of the poleyenes have one side that is highly lipophilic and has plenty of conjugated double bonds, and the other side that is hydrophilic and has lots of OH groups. Some have a polar aminosugar and a carboxylic acid group at one end. They are all soluble in water and unstable in watery media.
Mode of action of Nystatin:
A polyene macrolide antibiotic called nystatin works by attaching to sterols in the plasma membranes of fungi, causing the cells to leak and ultimately resulting in fungal cell death. Nystatin is prescribed to treat gastrointestinal tract, skin, and mucous membrane candidal infections.
Mode of action of Nystatin:
Since nystatin is a channel-forming ionophore, it works to treat disease by creating a pore that spans the fungal plasma membrane. When this pore forms, the permeability of the membrane is altered, allowing internal contents to leak out and disrupting the electrochemical gradients required for healthy cell function. Since ergosterol, a crucial sterol present in fungal cell walls, has a higher binding affinity than cholesterol in mammals, nystatin is more selective for fungal cells than mammalian ones.
Heterocyclic benzofuran
Griseofulvin
It was one of the early antibiotics extracted from Penicillium griseofulvum.
It is active against most dermatophytes including epidermophyton, trichophyton , microsporum but not against Candida and other fungi causing mycosis.
It is fungistatic in nature.
It interferes with mitosis-multinucleated and stunned fungal hyphae result from its action.
It causes abnormal metaphase configuration, however doesn’t cause metaphase arrest, rather the daughter nuclei fail to move apart or move only a short distance.
It does not inhibit polymerization of tubulin but somehow disorients the microtubules.
Antimetabolite
Flucytosine
It is a pyrimidine antimetabolite and inactive as such.
Flucytosine is taken up by fungal cells via the enzyme cytosine permease.
5-FC is then converted by a series of steps to 5-fluorodeoxyuridine 5’-monophosphate.
This false nucleotide inhibits thymidylate synthase, thereby depriving the organism of thymidylic acid, an essential DNA component.
The unnatural mononucleotide is further metabolized to a trinucleotide (5-fluorodeoxyuridine 5’-triphosphate) and is incorporated into fungal RNA, where it disrupts nucleic acid and protein synthesis.
Echinocandins
Echinocandins interfere with the synthesis of the fungal cell wall.
It is Glucan synthesis inhibitor.
It nhibits 1,3- beta glucan synthase, an enzyme important in fungal cell wall synthesis and subsequently inhibit the synthesis of beta glucan in the fungal cell wall.
Disruption of the fungal cell wall leads to cellular osmotic instability and cell death.
Terbinafine
It is synthetic allylamine and orally active.
It is used for treating dermatophytoses, especially onychomycosis.
It interferes with ergosterol biosynthesis by inhibiting the fungal enzyme squalene epoxidase rather than interacting with the P450 system.
Acting as a structural analogue of squalene, terbinafine causes the accumulation of this unsaturated hydrocarbon, and a decrease in ergosterol in the fungal cell membrane.
The accumulation of toxic amounts of squalene result in the death of the fungal cell.
Topical antifungals
A. Ciclopirox
Ciclopirox inhibits the transport of essential elements in the fungal cell, disrupting the synthesis of DNA, RNA, and protein.
Ciclopirox is active against Trichophyton rubrum, Trichophyton mentagrophytes, Epidermophyton floccosum, Microsporum canis, Candida albicans, and Malassezia furfur.
B. Tolnaftate
Tolnaftate distorts the hyphae and stunts mycelia growth in susceptible fungi.
Tolnaftate is active against Epidermophyton, Microsporum, and Malassezia furfur.
Allylamines
A similar enzyme involved in the formation of the fungal cell membrane is interfered with by allylamines, just like it is by azole antifungals. Terbinafine, which is frequently used to treat skin fungus infections, is one example of an allylamine.
Echinocandins
Echinocandins are a newer type of antifungal drug. They inhibit an enzyme that’s involved in the making of the fungal cell wall.
Some examples of echinocandins are:
Anidulafungin: mucosal and invasive Candida infections
Caspofungin: mucosal and invasive Candida infections, aspergillosis
Micafungin: mucosal and invasive Candida infections
Miscellaneous:
There are also some other types of antifungal medications. These have mechanisms different from the types we’ve discussed above.
Flucytosine is an antifungal that prevents the fungal cell from making nucleic acids and proteins. Because of this, the cell can no longer grow and thrive. Flucytosine can be used to treat systemic infections with Candida or Cryptococcus species. Griseofulvin works to prevent the fungal cell from dividing to produce more cells. It can be used to treat infections of the skin, hair, and nails.
Fungal infections:
There are many types of fungal infection. You can get a fungal infection by coming into contact with a fungus or fungal spores that are present in the environment. Some of the most common fungal infections are those of the skin, nails, and mucous membranes. Examples include: Ringworm: a fungal infection of the skin that can occur on your scalp, on your feet (athlete’s foot), in your groin area (jock itch), and on other areas of your body
Nail fungus: an infection that typically affects your toenails but can also affect your fingernails
Vaginal yeast infection: an infection that occurs due to overgrowth of Candida yeast in and around the vagina Oral thrush: a condition in which Candida yeast overgrows in your mouth
More serious fungal infections:
There are also some less common but more serious fungal infections that can cause fungal pneumonia, fungal meningitis, or even systemic infections.
Examples of fungal species that can cause more serious infections include:
Aspergillus
Blastomyces
Candida
Coccidioides
Cryptococcus
Histoplasma



Comments
There are no comments for this story
Be the first to respond and start the conversation.