AI Predicts 96% of COVID-19 Pneumonia Cases Which Will Require Intensive Care.
Coronavirus Treated by A. I System in Future
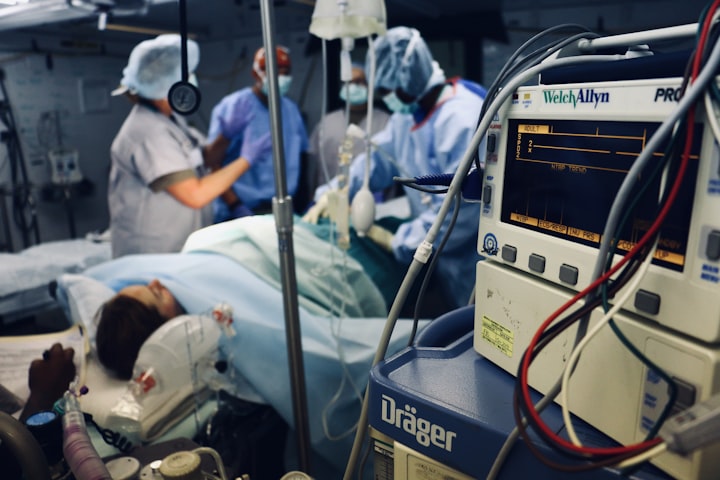
As intensive care units hit capacity in many parts of the world, physicians have to make hard decisions about who receives a mattress amid a worldwide pandemic.
Now, a new machine-learning algorithm could help us figure out who is most at risk, so we can intervene early and hopefully save their own lives.
The algorithms hunt the tests for lung abnormalities and discover COVID-19-related pneumonia in roughly 90 percent of instances.
These scans can't tell us with nearly as much accuracy how severe those instances might become and who's the most vulnerable.
The new algorithm takes matters a step further by mixing chest scans with non-imaging data, including demographic information, vital signs, and blood work. And it is the best we've up to now at predicting when someone needs ICU intervention.

The strategy has only been analyzed using health data from 295 patients hospitalized for COVID-19 either in the United States, Iran, or Italy. But even in these early stages, it was able to predict as many as 96% of COVID-19 cases that would require ICU admission, based on the preprint paper.
"As a professional of AI, I do believe in its ability," says engineer Pingkun Yan from Rensselaer Polytechnic Institute.
"It really enables us to examine a massive amount of information and also extract the features which may not be that obvious to your eye."
During a global pandemic, that type of insight is invaluable and potentially life-saving. Those who create the most acute cases of COVID-19 pneumonia should have several common attributes; finding the right ones is a lot quicker for a smart machine than it is to get a human.

Machine learning programs have been used to evaluate which signs are most likely to forecast COVID-19 mortality.
Initial findings suggest ventilator usage and potassium levels are the most significant non-imaging factors. However, other contributors also have been identified, including lymphocyte percent, total bilirubin, creatinine, and albumin levels, to mention a few.
The new algorithm moves a step farther:
1. It quantifies the scope and volume of lung features.
2. It targets those attributes which are most significant in calling COVID-19 pneumonia.
The group expects further refinement. One day, the instrument may be used to screen for high-risk patients with COVID-19 pneumonia, who require closer monitoring and care.
While the team didn't test how COVID-19 pneumonia contrasts with other respiratory diseases, the broad similarities in lung distress imply the algorithm might prove beneficial even when the pandemic is over.
"We actually are seeing that the impact could go well beyond COVID ailments. By way of example, patients with other lung diseases," Yan says.
"Assessing their heart disease condition, in addition to their lung ailment, could better forecast their mortality risk so that we can help them manage their ailment."
Other intensive care management
Patients with COVID-19 may have hypovolaemia because of anorexia, vomiting, and diarrhea.
Nevertheless, fluids should be treated carefully, and preferably with assessments for pre-load responsiveness such as the passive leg raise test, given the high prevalence of esophageal dysfunction in COVID-19.
This incidence may be a result of the strong binding affinity of this SARS-CoV-2 spike protein into human angiotensin-converting enzyme 2 (ACE2), a membrane-bound receptor crucial for host cell entrance that's expressed in the lungs and heart, among other organs.
A traditional or de-resuscitative fluid strategy,
And early use of vasopressors and inotropes are recommended.
Most sufferers with COVID-19 in China have been granted empirical broad-spectrum antibiotics and many, oseltamivir because lab analysis of COVID-19 takes time, and differentiating the disease from other bacterial and viral pneumonia is often difficult.
One study of 201 patients using COVID-19 found just 1 co-infection using a different virus and none with bacteria. Another analysis of 92 patients discovered six co-infections by other common respiratory viruses, along with a third study of 115 patients discovered five co-infections with influenza. Any empirical antibiotic and also anti-influenza therapy ought to be rapidly de-escalated based on microbiology test results and clinical reaction.
Chinese reports also demonstrate that systemic corticosteroids were administered to approximately half of individuals using COVID-19 with serious or significant illness.
A retrospective study of 84 patients with ARDS associated with COVID-19 found lower mortality in people treated with methylprednisolone, but the findings are limited by the observational design of this study, small sample size, and possible confounders.
Because COVID-19 might be related to a cytokine storm like that seen in other viral diseases, immunosuppression has been proposed as an approach that might be good for patients with signs of hyper inflammation, such as raising ferritin concentrations.
Likewise, an observational study found that corticosteroids for MERS didn't have an effect on mortality but did postpone viral clearance.
Until further data are available, the routine use of corticosteroids in viral severe acute respiratory ailments, including COVID-19, isn't advised.
Quick liberation from invasive mechanical ventilation to reduce the incidence of ventilator-associated pneumonia and to make ICU capacity must be balanced against the risks of premature extubation (particularly without facilitative post-extubation NIV and HFNC) and subsequent re-intubation (along with the attendant risks of viral transmission to health-care employees). Transfer of patients out of the ICU for investigations such as CT scans dangers spreading SARS-CoV-2 and may be minimized with options like point-of-care ultrasound.
The latter was prioritized by some Western ICUs, and evidence of varying degrees of an interstitial pattern and consolidation on lung ultrasonography currently exists for patients with COVID-19.
WHO recommends that de-isolation of sufferers requires clinical retrieval and two negative RT-PCR assays performed 24 h apart.
This fact has significant implications for the use of isolation facilities.






Comments
There are no comments for this story
Be the first to respond and start the conversation.