A new study found that removing both ovaries surgically can cause long-term health complications in women who have not yet reached menopause.
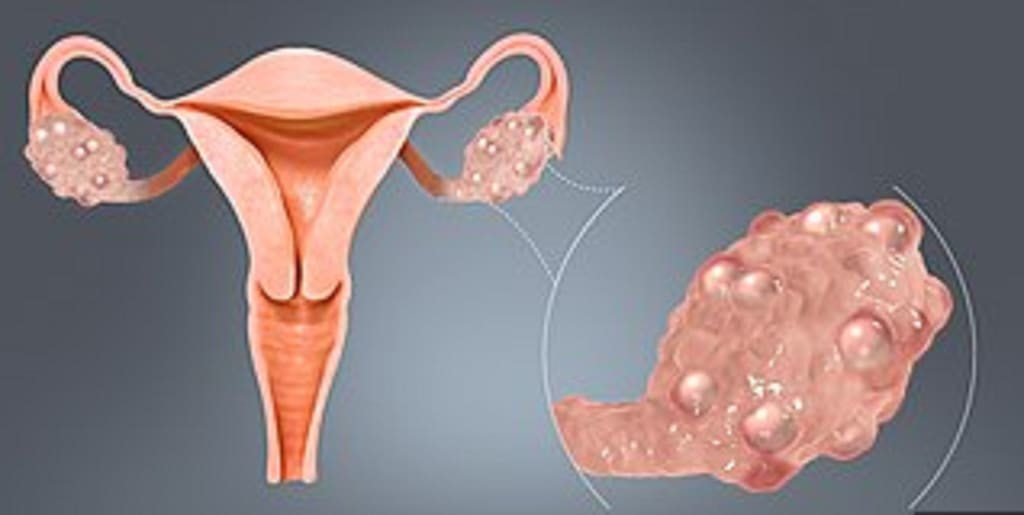
This procedure, known as a premenopausal bilateral oophorectomy (PBO), is commonly performed as part of a hysterectomy. They may also recommend it to high-risk individuals to reduce their risk of ovarian cancer.
In individuals who are not at a high risk for ovarian cancer, however, ovary excision before menopause is often unnecessary and can cause long-term health problems, according to an increasing number of experts.
Michelle Mielke, PhD, a professor of epidemiology and prevention at the Wake Forest School of Medicine in Winston-Salem, North Carolina, and the study's lead author, states that the objective of the new research is "to give women more control over their health and the ability to weigh the pros and cons of having their ovaries removed."
She notes that the risk-benefit analysis will differ for women with a greater likelihood of developing ovarian cancer.
Scientists Warn of 'Detrimental' Effects
In the study, published in the journal Menopause on September 13, 2023, Dr. Mielke and her colleagues compared the medical records and cognitive tests of more than 500 Minnesota women residing in the same county. The remaining half had not undergone a PBO with or without hysterectomy.
The median age of women who had undergone PBO was 67, and they had, on average, undertaken the procedure at least 22 years prior to the study's inception. Participants with remaining ovaries were at least 55 years of age.
The researchers discovered that subjects who had both ovaries removed prior to the age of 46 had an increased risk of developing osteoarthritis, asthma, obstructive sleep apnea, and bone fractures. Those who had a PBO between the ages of 46 and 49 were more likely to develop arthritis and sleep apnea.
The researchers found no differences in cognitive function between those who had their ovaries removed and those who did not, nor between the ages of the PBO group.
"We have known for generations that removing a woman's ovaries before menopause is extremely detrimental for many different areas, including how the heart and bones function," says Elena Ratner, MD, professor of obstetrics, gynecology, and reproductive sciences and co-chief of the section of gynecologic oncology at Yale University School of Medicine in Connecticut, who was not involved in the new study.
"However, there are certain groups of women for whom we accept this disadvantage in order to reduce their risk of ovarian cancer," she continues.
Ovary Extraction Is Common Following Hysterectomy
In addition to cancer prevention or birth control, a woman may choose to have a hysterectomy if she has uterine fibroids or uterine prolapse, endometriosis or adenomyosis, or excessive or unusual vaginal bleeding, according to the U.S. Department of Health and Human Services' Office on Women's Health.
According to Yale Medicine, hysterectomy is the second most common surgery for women, after cesarean section, with approximately 500,000 hysterectomies performed annually. The authors of the study estimate that one-fourth of women aged 40 to 44 and nearly half of women aged 45 to 59 who have had a hysterectomy have also had their ovaries removed.
"Removing the ovaries during a hysterectomy has been a common procedure," says Mielke. Now, research suggests we should reconsider this. If a patient undergoes a hysterectomy, it may be prudent to retain the ovaries."
Why Does Ovariectomy Affect the Heart and Bones?
In addition to producing and storing eggs, ovaries also produce the essential hormones estrogen, progesterone, and even a small quantity of testosterone. In addition to regulating the menstrual cycle and pregnancy, these hormones play extensive functions throughout the body, particularly in relation to the cardiovascular system and bones.
According to the American College of Obstetricians and Gynecologists (ACOG), estrogen decline causes a rapid decrease in bone density. ACOG reports that the hormone also has a protective effect on the cardiovascular system.
Natural menopause has been linked to higher rates of cardiovascular disease and osteoporosis, in part because estrogen levels decline. Surgical menopause — menopause induced by the removal of the ovaries, frequently before the onset of natural menopause — seems to have an even greater impact.
"During menopause, there is a gradual decline in hormone levels, but with PBO or hysterectomy, it's a shock, a sudden drop," says Mielke.
A Danish study of more than 285,000 women, published in May 2023 in the Annals of Internal Medicine, found that women who had their ovaries removed before age 45 were more likely to be hospitalized for cardiovascular disease than women who still had their ovaries and those who had their ovaries removed later in life. These women also had a higher 10-year cumulative risk of cardiovascular hospitalization. In addition, their overall cancer risk increased after age 45, whereas their (average) ovarian cancer risk decreased.
People at High Risk for Ovarian Cancer Must Perform a Special Calculation
Those with a high risk of ovarian cancer must weigh the benefits and drawbacks of having their ovaries removed before menopause as a preventative measure.
"Ovarian cancer remains lethal due to the fact that women are typically diagnosed at an advanced stage." "It's not for lack of effort that we fail to detect these cancers early," says Mielke.
Mielke and Dr. Ratner concur that ovarian cancer is challenging to detect with an ultrasound, and that there is no reliable blood test for the disease. For these reasons, prevention has always been the most effective strategy.
Mielke encourages all women to undergo genetic testing to identify mutations that place them at increased risk for ovarian cancer. Then, she says, they can better evaluate their options.
Ratner suggests that removing the ovaries or, conceivably, just the fallopian tubes (which connect the ovaries to the uterus) may be the best course of action for individuals at high risk for ovarian cancer, including those with genetic mutations such as BRCA or a family history of cervical cancer.
Ratner states that many ovarian cancers are essentially cancers of the fallopian tubes. And since their only function is to facilitate natural conception, removing the uterus and fallopian tubes, but not the ovaries, from a woman who does not intend to become pregnant is another option for reducing cancer risk while preserving the ovaries.
Ratner explains that hormone therapy can mitigate some of the side effects of PBO if it is the best option for a woman who is at high risk for cervical cancer or has another condition that necessitates ovary removal.
"We do recommend ovary removal for women who are indeed at high risk for ovarian cancer," she says.
About the Creator
Mr Henry
I strive to create engaging and thought-provoking content that captivates readers. I aim to evoke emotions, spark curiosity, and inspire others. I am dedicated to honing my skills and continuously improving as a writer






Comments (2)
Good one
Very interesting! Fantastic work!