I started posting on Vocal with a goal of at least one post a week but I have already missed at least two weeks. I can’t tell you exactly why because I don’t have a name for it yet. The doctors know that I have a second autoimmune disease and that it is possibly attacking my nerves. I recently got a working diagnosis debunked but this isn’t the first one. The process of diagnosis can be long and painful. In the meantime, without knowing what is wrong with you, adjusting and asking others to adjust is difficult. With autoimmune disease, it almost never is an easy diagnosis, or even a difficult but quick House M.D. style one. This puts extra stress and anguish on those who are suffering. I have already told one of my own stories so I wanted to take a wider look at the problem.
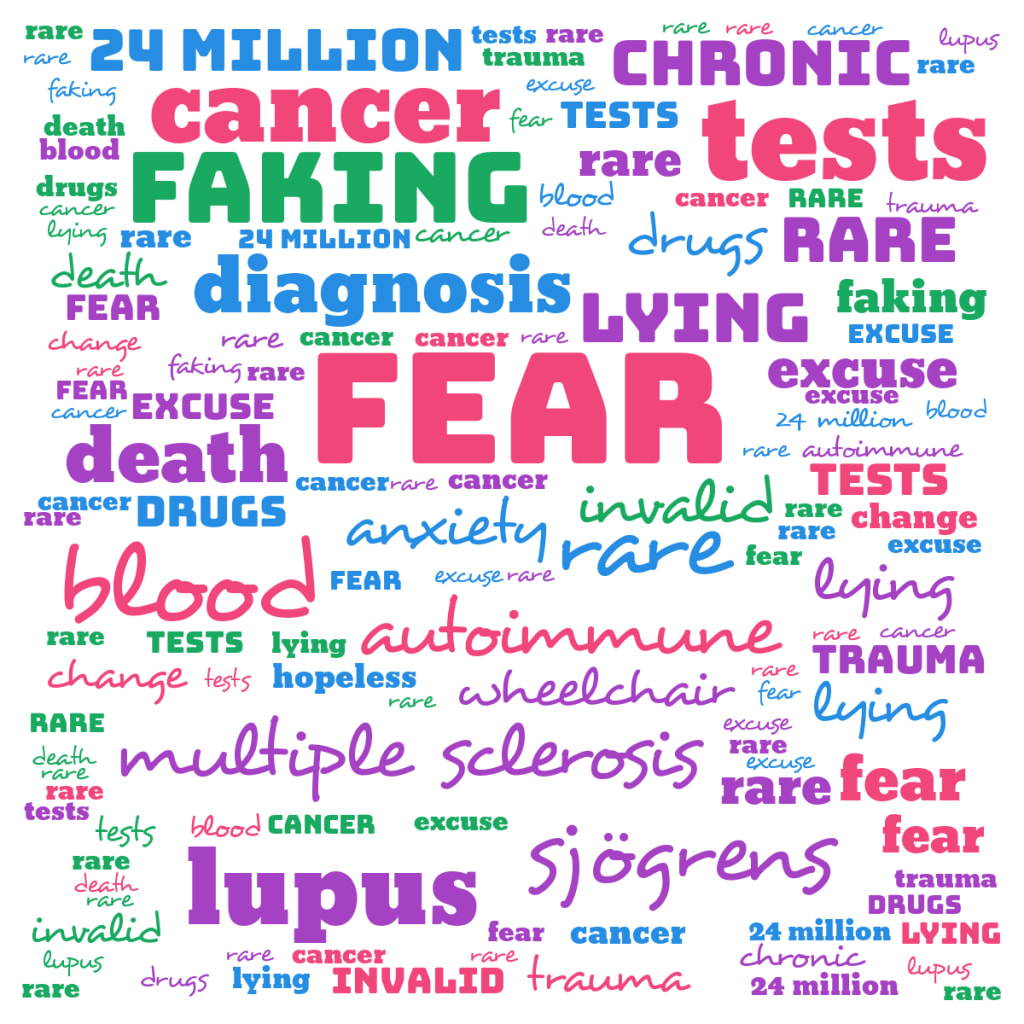
I am not a doctor and a lot of what’s below is my personal experience and commentary. However, I feel it would be irresponsible not to include some medical grade information. According to the National Institute of Environmental Health Sciences, part of the NIH, the rarity of certain AIs (autoimmune diseases) makes them difficult to diagnose. They admit that for these, it can take years to diagnose. They also say that there are over 80 known AIs and that over 24 million Americans alone are affected. Yet still, a lot about AIs remains unknown.
The University of Virginia Health System blog spoke to a rheumatologist about the difficulty of diagnosing AIs. According Dr. Angela Crowley, “People on average see six doctors over a period of four years before they get a diagnosis” (Marshall). She lists many reasons for this but I have personal experience with mimics, co-conditions, and delayed symptoms.
Mimics are diseases that share signs and symptoms, leading doctors astray. These include lupus and MS, and CIDP and small fiber neuropathy. I have had scares of all of these and cannot say for sure that they are completely ruled out. And I have been tested for two of them, told there was a high chance. Of course, this lengthens the diagnosis process but it also causes a lot of patient anxiety and confusion. They’re told, or it is suggested that, they likely have (insert scary, life altering disease here) and sent to have more blood taken or get a medical scan. In the meantime, they try to get a grasp on the condition and prepare themselves emotionally for the impending diagnosis and treatment. They go in, after waiting weeks, and find out the test was negative. Whoo hoo! They don’t have X but they also don’t have answers.
Co-conditions also can confuse doctors and patients. As mentioned in the UVHS article, Celiac disease, and other AIs, can lead to, or co-exist with, any other AI or other disease. When one is diagnosed, both patient and doctor may think that is all that is going on. Celiac often occurs with other conditions as it has for me. I was diagnosed in August after ten years of weird symptoms and very low iron. I was told by my well meaning GI that I would feel so much better once going gluten free and getting iron infusions. But no, before my infusions, my iron continued to drop and I ended up in a hospital bed with someone else’s blood flowing through me at three a.m.. Despite being gluten free and having normal iron, some of my old symptoms are still present and I have new ones. I wish I had more tests done back in August, before it got worse and I became terrified, but how was anyone to know that something else was going on when Celiac explained my symptoms at the time? Was it even going on then? I don’t think there is any way to know for sure.
That leads me to delayed symptoms. An AI, or other disease, can be active in the body, doing damage, for a long time before any symptoms are noticed. With Celiac, I did not have severe GI symptoms until this past summer and those were key for my diagnosis. For some diseases, doctors may look for “tell-tale signs” like reflex changes with MS or a butterfly rash with lupus. But these specific signs don’t have to appear right away or at all. Someone can go years with lupus symptoms and anxiety over them and one day wake up with a butterfly rash that, had they had it at the start, would have led to a diagnosis much sooner.
But the diagnosis process of AIs does not just impact me or some hypothetical person. The University of North Carolina’s Department of Medicine interviewed a woman named Kristen about her experience. I highly suggest listening to the whole thing but here are some parts that I found particularly salient.
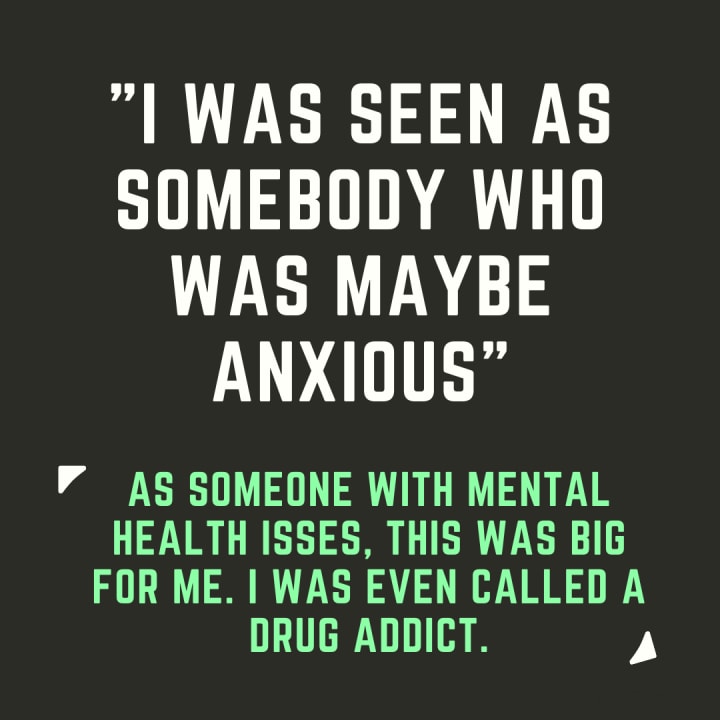
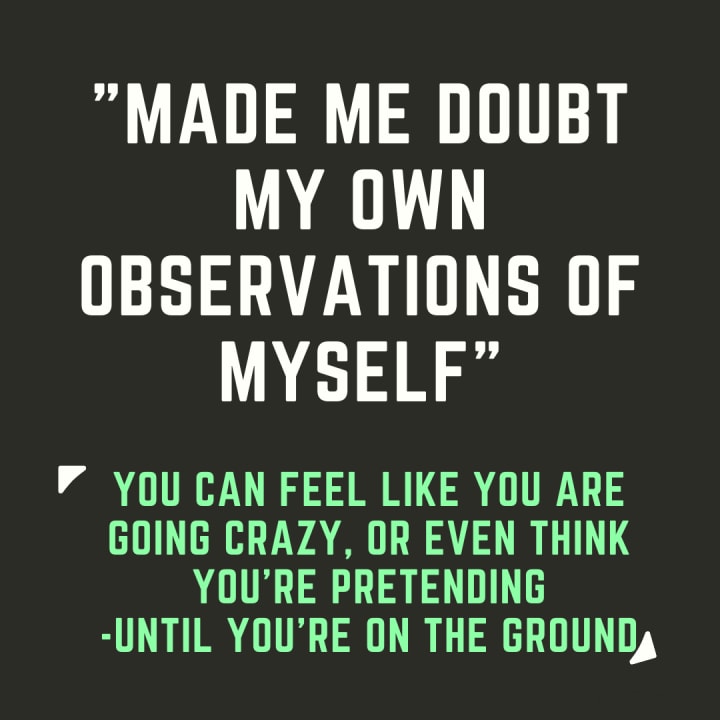
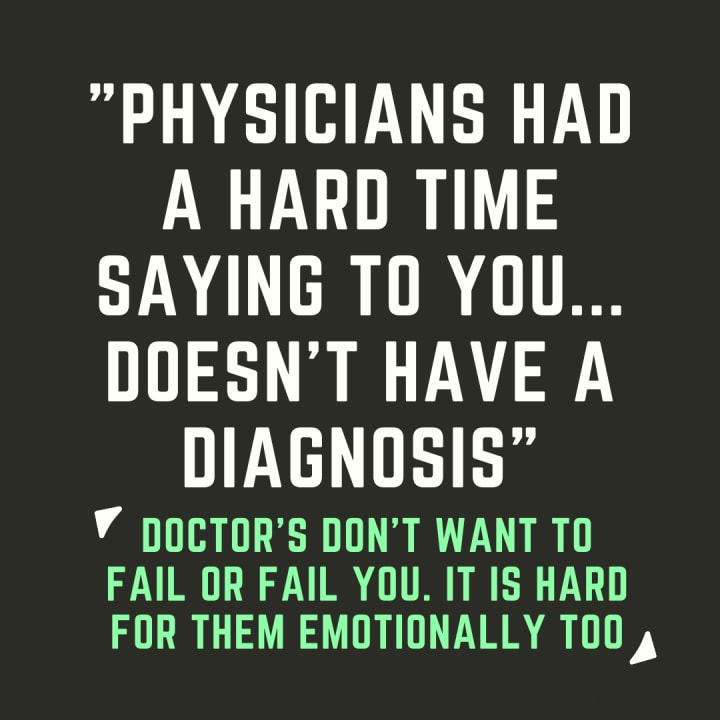
I think it’s pretty clear that the diagnosis process of autoimmune diseases can have some intense mental health impacts, along with the physical. Obviously, not knowing what’s wrong with you, and not getting treatment, can cause massive amounts of anxiety. This anxiety can impact other parts of your life such as your social or work life. Being stuck in the process also causes a fair amount of guilt. You can’t do certain things and yet, to some, you don’t have a valid excuse. You’re seen as bailing and slacking. This impacts your self confidence and can even mess with your feeling of sanity. You feel pain but people say there’s nothing there. It is the definition of maddening. Unfortunately, this process also heightens your chances of experiencing medical trauma which could leave you with PTSD or other trauma related issues. This is not a simple problem or even a purely temporary one. The damage from a long diagnosis period can be permanent. If you are in the process, don’t be afraid to reach out for help coping.
And doctors, please understand, a patient being upset does not mean they are faking, or that the problem is in their head. They are terrified, not knowing what they will and won’t be able to do in the next days, weeks, and months, not knowing if they are dying, not knowing how their life is changing or why. It is a horrible position that too many people are in.
Researchers, I personally don’t think that curing individual AIs should be the main focus of study, understanding all of them together is extremely crucial. When doctors are able to diagnose and treat quickly, patients will have so much more peace of mind along with the tools to keep going.
About the Creator
Jade Neal
I'm a performer, diplomacy student, and chronic illness survivor. I'm here to share my story and knowledge in order to help someone out or provide entertainment.





Comments
There are no comments for this story
Be the first to respond and start the conversation.